Reddit cofounder Alexis Ohanian calls this ‘the highest ROI $100 you can spend on your health.’ Here’s what to know about the calcium score test’s benefits
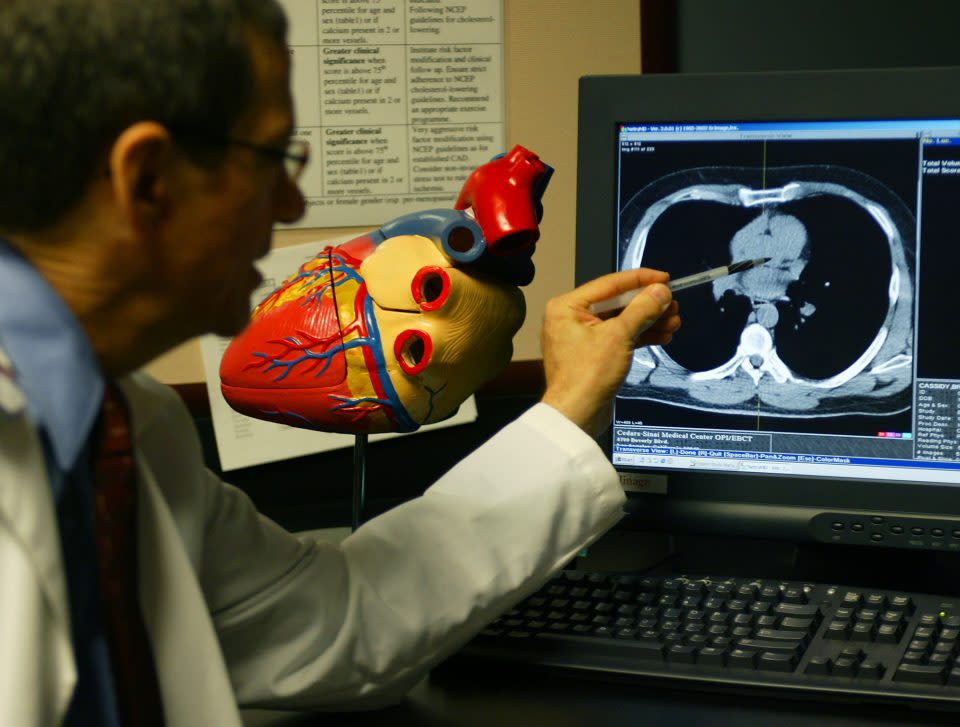
Last year, Reddit cofounder Alexis Ohanian underwent a medical procedure he now lauds as a relatively inexpensive health investment: a calcium score test. It’s a type of computed tomography (CT) scan known by several names, including a coronary calcium scan. The American Heart Association calls it a CAC test, short for coronary artery calcium.
By providing a “calcium score” based on the level of calcium buildup in your coronary arteries, a CAC test is used to help determine your risk of heart disease, heart attack, and/or stroke. The noninvasive scan can detect early-stage coronary artery disease, typically before symptoms develop.
Last week, Altimeter Capital founder and CEO Brad Gerstner posted on X (formerly Twitter), “Get a Calcium CT Scan of your arteries - $100 / 30 mins can save your life.” Ohanian quoted the post, adding, “I did this last year. Probably the highest ROI $100 you can spend on your health.”
When plaque builds up in the blood vessels that feed your heart, a process called atherosclerosis, chest pain, or a heart attack may result, Dr. Joseph Ebinger, associate director of the Coronary Intensive Care Unit at Cedars-Sinai Medical Center in Los Angeles, tells Fortune. The blockage begins as soft plaque, made up of cholesterol deposits and other substances. But in an attempt to “wall off” the soft plaque, your body eventually develops calcium around it, Ebinger explains.
“Calcium is like a bone-type material—it’s really hard,” Ebinger tells Fortune. “That shows up on noncontrast CT scans and allows us to be able to quantify the amount of calcium that’s built up on the coronary arteries.”
He adds, “There are very clear epidemiologic studies that have shown a relationship between the presence and the degree of coronary artery calcification and the risk of future cardiovascular events.”
I did this last year. Probably the highest ROI $100 you can spend on your health. https://t.co/k45vgLGsBj
— Alexis Ohanian 🇦🇲 (@alexisohanian) March 3, 2024
Should I get a calcium score test?
It may be helpful to think of the CAC test as a Goldilocks procedure; it’s designed for people at not low or high, but moderate risk of cardiovascular disease.
“If you have a super-low risk because you are 25, never smoked, have well-controlled cholesterol, your risk of a cardiovascular event is really low. [A CAC test] is not going to help you,” Ebinger tells Fortune. “That said, if you are 70 and you have high cholesterol, you are a smoker, and you have high blood pressure, coronary calcium scanning is not going to help you a lot either… I’m going to treat you as if you’re high-risk.”
A CAC test won’t provide additional insight for patients who have already had a heart attack, coronary stent, or coronary bypass surgery, according to the American Heart Association (AHA). In addition, repeat testing isn’t beneficial for people who have gotten abnormal results in the past.
The AHA urges people to become familiar with their likelihood of a heart attack, including these “traditional” risk factors:
Diabetes
High blood pressure
High cholesterol
Overweight or obesity
Smoking
“Risk-enhancing” factors include:
Chronic inflammatory conditions
Chronic kidney disease
Family history of early atherosclerotic cardiovascular disease
Younger than 55 in men
Younger than 65 in women
High-risk ethnicity
Heart disease risk is higher among American Indian, Mexican American, native Hawaiian, and some Asian American people
Black people have disproportionately high rates of more severe blood pressure, which they develop earlier in life
Higher-than-normal triglycerides, ankle-brachial index, and other lab tests
History of preeclampsia or early menopause
Increasing age
Male gender
People between the ages of 40 and 75 who haven’t had a heart attack should ask their doctor to assess their 10-year risk of a cardiovascular event, the AHA recommends. CAC testing may then help physicians develop treatment plans for patients at intermediate risk.
Dr. Luke Laffin, a preventive cardiologist at Cleveland Clinic, suggests speaking to your primary care physician about your risk factors and whether a CAC test may be appropriate—even if you’re on the younger side like Ohanian, 40.
“It’s a field in flux, and I think most preventive cardiologists are moving toward being a little bit more aggressive with coronary calcium scoring in younger, lower-risk patients,” Laffin says. “It doesn’t mean everyone should get it, but it has to be an individualized decision based on family history and other risk factors.”
While both Gerstner and Ohanian said they spent $100 on their CAC tests, the AHA notes the procedure isn’t always covered by insurance and can range from $100–$400.
Calcium score test is a tool, not a testament
A CAC test is one you want to fail; a score of 0 means you don’t have any calcified plaque in your coronary arteries, and/or you have a very low short-term risk of stroke or heart attack, Laffin says. The scans are graded on what’s called an Agatston score:
0: No identifiable disease
1–99: Mild disease
100–399: Moderate disease
Over 400: Severe disease
But just as a high score isn’t a death sentence, a low score provides your doctor with only a piece of the puzzle. For example, a CAC test doesn’t show the degree of blockage or narrowing in an artery, Laffin says.
“It’s a biomarker, like blood pressure, like cholesterol,” Laffin tells Fortune. “If it’s elevated—greater than 0—it suggests that there’s already plaque within those arteries, and we should be aggressive about trying to control cardiovascular risk factors.”
Ebinger calls the CAC test “a fine-tuning mechanism.” While you’re stuck with some risk factors such as age and heredity, focus instead on what you can modify, such as getting your cholesterol under control, Ebinger says. Your doctor may recommend a statin, a type of prescription drug used to lower “bad” (LDL) cholesterol, based on your CAC test results.
In his X post, Gerstner wrote, “Well intended cholesterol charts have mis-led millions of people about heart disease. Cholesterol is NOT a predictor of heart attacks - approx 50% of heart attack patients have LDL levels in the green!” He included a cholesterol chart that notes total cholesterol under 200 is heart-healthy, which appears to have been copied from the Cleveland Clinic website. Gerstner didn’t say where he got his numbers; conversely, a 2023 AHA survey found that 75% of heart attack and stroke survivors reported having high cholesterol.
Like the CAC test, cholesterol level is just one tool to help paint a picture of your overall health and cardiovascular disease risk, Laffin says, noting that LDL cholesterol is perhaps a more valuable measure of risk at the population level.
Gerstner, 52, said on X that his concierge doctor cited his “great health” as a reason not to get a CAC test, “But I insisted bc I have had too many friends die young of heart attacks.” Gerstner scored a 77, indicating mild heart disease and spurring him into action.
“The discovery of plaque led me to 1) get a CT Angiogram / Heartflow which found below avg uncalcified plaque / limited blockage (good news) 2) take a statin / ezetimibe which has reduced my LDL to 36,” Gerstner wrote. “I am now preventing the build up of addt plaque and have a baseline to monitor and avoid problems. Living without data is NOT a strategy!”
Gainsight CEO Nick Mehta responded, “I had the exact same experience. Great cholesterol but still had blockage. On statins now.”
For more on CEO wellness:
This story was originally featured on Fortune.com
