In rare cases COVID-19 can cross placenta, causing fetal brain damage, UM study says
In rare cases, COVID-19 can be passed from a pregnant mother to her fetus, researchers at the University of Miami Health System and the University of Miami Miller School of Medicine announced Thursday.
The team’s study published April 6 in the journal Pediatrics, “Maternal SARS-CoV-2, Placental Changes and Brain Injury in Two Neonates,” found that, in two cases, the novel coronavirus infection breached the placenta and caused brain damage in the newborns.
“COVID not only affects the mother herself, but also puts the unborn baby at risk,” said the study’s lead author, Dr. Merline Benny, a UHealth assistant professor of pediatrics and neonatologist.

What happened to the babies
The two babies were admitted to the Neonatal Intensive Care Unit at Holtz Children’s Hospital at University of Miami/Jackson Memorial Medical Center, a teaching hospital affiliated with UHealth and the Miller School, in 2020.
After the babies were born, both infants experienced seizures, had small head sizes and developmental delays. One infant, a Hispanic boy born by Cesarean to a 21-year-old mother, died at 13 months, three days after returning to the hospital with a respiratory infection. The infant died at home in cardiac arrest. Paramedics could not revive the child, the study said.
The second baby, a girl, also Hispanic, was born vaginally and her mother was 20 years old when she delivered.
According to the study, at a checkup at age 1 year, the surviving child showed microcephaly, a condition in which a baby’s head is smaller than normal, according to the U.S. Centers for Disease Control and Prevention. That baby also had an abnormal neurologic examination with significant neurodevelopmental delays and an inability to roll over or sit unsupported. The infant is currently in hospice care, according to the study.
What the study found
According to UM, this is the first study to confirm cross-placental SARS-CoV-2 transmission leading to brain injury.
“We have had nearly 700 and more mother-infant pairs in the Jackson hospital who were admitted and all these mothers who were COVID positive, the majority of them were asymptomatic. And even the infants, the majority of them, were very healthy after delivery and left the hospital without any complications,” Benny said.
“However, here we report in this study two babies who had a very unusual clinical picture,” she said during a Zoom call Thursday to announce their findings. “These infants were born to mothers who were COVID positive who became positive in the second trimester of their pregnancy and delivered a few weeks later. Neither of these babies however, tested COVID positive. However, in their blood, we found that the COVID antibodies were present, which suggests that the COVID antibodies must have crossed from the mother to the placenta to the baby.”
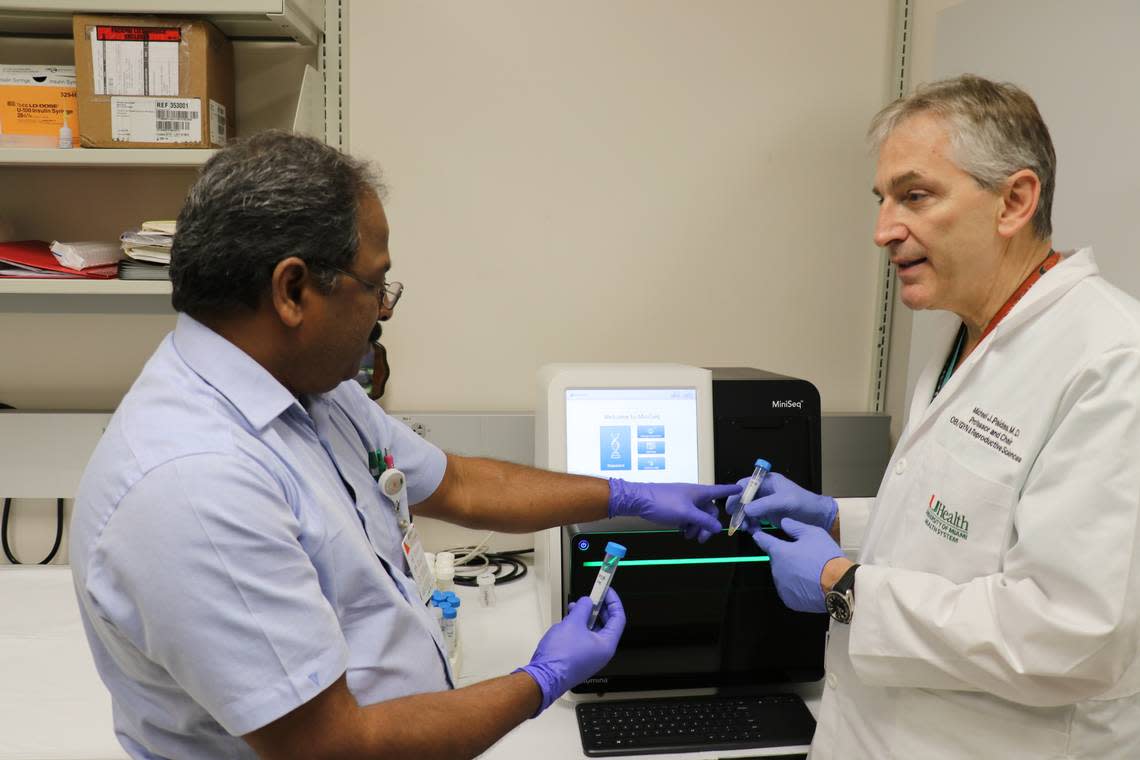
The medical team stressed that the two mothers were pregnant in 2020 before the availability of vaccines, said Dr. Michael Paidas, professor and chair of the Department of Obstetrics, Gynecology and Reproductive Sciences at the Miller School and Jackson’s chief of service for obstetrics and gynecology.
COVID variant subtypes were not a part of the study.
“It is hard to know whether variant subtype is the critical factor, especially since the data regarding disease severity in pregnancy is somewhat contradictory regarding subtypes. I don’t think it is the variant subtype as much as the viral load, and other factors such as the degree of inflammation, thrombosis, vasculopathy and the presence of other co-morbidities,” Paidas told the Miami Herald.
“We need to continue our research to figure out why these two babies experienced such devastating results,” Benny said.
Clearly unusual outcomes
“Many women are affected by COVID-19 during pregnancy, but to see these kinds of problems in their infants at birth was clearly unusual,” said Dr. Shahnaz Duara, a professor of pediatrics at the Miller School of Medicine and the medical director of the Neonatal Intensive Care Unit at Holtz, a senior author on the study. “These babies were strikingly different. We have absolutely no good explanation for the early seizures, and the degree of brain injury. They were not infectious. There was no issue during labor. And we investigated every avenue.”
Duara said what stood out were the elevated antibodies tied directly to the COVID virus and inflammatory markers.
“That’s when we began to talk to our pathologists, we started talking to the neuroradiologists who did not see the signatures of other injuries, and we went back to our obstetricians. So it sort of was a little bit of a detective story. We’re trying to understand what made these two pregnancies different so we can direct research towards protecting vulnerable babies,” Duara said.
“I think the message here is that most women who contract COVID go on to have healthy babies. But there is a sub-population of people who have babies who are sick. And so this is not to panic the population whose babies may have been exposed to COVID in pregnancy. But we do think that these are the extremes and we do think if you’ve had COVID during pregnancy, it’s something you should tell your pediatrician, and maybe those babies need a little closer follow-up,” Duara said.
According to UM, in 2020, early during the COVID-19 pandemic, this group of neonatologists had observed transient lung disease and sometimes blood pressure issues among newborns who had similarly tested negative at birth but were born to COVID-19 positive mothers. It was left unclear “whether the SARS-CoV-2 virus crossed the placenta and injured the baby.”
But Paidas said it wasn’t a lack of blood flow to the placenta that caused these two infants’ problems. “As best we can tell, it was the viral infection.”

How to protect baby
During the Zoom conversation, the study’s authors stressed the importance of maternal COVID-19 vaccination as a line of defense.
“It is important for us to get the message out that it is not always benign. A lot of young people who are in the reproductive age group see COVID as a nuisance. ‘It doesn’t matter. I can go to a rock concert and expose myself, not take vaccines, and I’ll be OK.’ You probably will be OK. But there is going to be a proportion of pregnant women who will expose themselves and may not have the consequences they anticipated,” Duara said.
Adds Paidas: “Vaccines have been shown to be safe and they will afford some protection for pregnancy. So I would encourage that. And secondly, the urgent need to develop therapeutics for our vulnerable populations, for moms and newborns, and adolescents. So we need more research and we need more patient engagement in the clinical trial arena. And finally, we need a longer term follow-up.”
