As polio reemerges in New York, here’s what to know about polio and its risk in Florida
“Even a single case of polio is a threat,” opined New York State Health Commissioner Mary T. Bassette in an op-ed essay in The New York Times on Aug. 21.
“The case of a young adult paralyzed by polio in New York is not simply unexpected. It’s shocking,” she wrote exactly one month after a 20-year-old unvaccinated man contracted the disease.
Polio may have been circulating in New York even longer, given that it was present in New York’s wastewater in April, according to a new report from the Centers for Disease Control and Prevention.
“Sustained poliovirus transmission has been eliminated from the United States for approximately 40 years,” according to the CDC. “The last time polio was diagnosed in New York State was in 1990,” Bassette wrote.
“We will learn more, but what we know already is enough. We have circulating poliovirus that can cause paralysis in these communities. Polio in New York today is an imminent threat,” she wrote.
But if polio is a worry in New York City is it a worry in Miami? We are, after all, sister cities. “Changes in the genome of the virus suggest that this version has been circulating, somewhere in the world, for up to a year,” New York Times reported in August.
Are we in Florida in the “somewhere?” category?
The Miami Herald reached out to Dr. Mary Jo Trepka, a professor and chair of Florida International University’s Department of Epidemiology at the Robert Stempel College of Public Health & Social Work. We asked her to help answer some questions you may have concerning polio and whether we ought to be concerned in the Sunshine State.

Is polio in Florida?
As of Sept. 3, there are no reported cases in Florida this year, according to the state health department’s reportable diseases frequency report. There have only been two in Florida since polio was declared eradicated in the U.S. in 1979 — in Hillsborough in 1996 and Orange County in 1997, according to the chart.
Is there a particular risk of polio in Florida?
What would make us susceptible, we wondered?
“The risk of polio, as with other vaccine-preventable diseases such as measles, mumps, rubella, diphtheria and pertussis, principally depends on the underlying level of vaccination in the community,” Trepka said.
Trepka said that Florida’s vaccination rate among kindergarten students at 93.3% in 2020-2021 is slightly lower than that of the U.S. as a whole, which was at 93.9%.
There was a slight downturn from 2019-20 — 93.5% — coinciding with the spread of the novel coronavirus and the introduction of COVID-19 vaccines, which for some have become politicized and polarizing.
“The pandemic has led to lower vaccination rates in many people,” Trepka said. “Some states are doing better and others worse.”
The SchoolVaxView Interactive School Vaccination Coverage chart from the CDC finds that New York’s level of vaccinated kindergarten children is higher than Florida’s rate — 97.8% compared to 93.4%.
“But the person with the case of polio, who was unvaccinated, lives in a county (Rockland) with a very low vaccination rate. That can happen here, too. By that I mean there may be small communities within Florida with lower vaccination rates than the overall state rate. In such groups of people, we see outbreaks,” Trepka said.
Polio affects children younger than 5 more than other age groups, according to the Mayo Clinic.
Is Florida’s wastewater a risk factor?

Polio was seen in wastewater in New York, much like COVID is detected in wastewater around the country, including in Florida. After a good rainstorm, and it doesn’t have to be a tropical system or hurricane, some of our streets as in downtown Miami and Brickell Avenue flood. You may be wondering, hmmm?
“In order to get polio from flooding, there would have to be contamination of the water by sewage from people who were infected with polio and you would have to ingest that virus,” Trepka said. “One way that could happen would be to contaminate your hands and subsequently contaminate food you eat. Given that we have not had a case of polio reported in Florida for more than 10 years, exposure to polio would be unlikely at this time. In Pakistan, where there is a much larger problem with polio and where there are massive floods now, the risk is clearly higher.”
Miami-Dade County is doing surveillance for the SARS CoV2 virus, the virus that causes COVID-19, in its wastewater. “Surveillance for poliovirus could potentially be added as is happening in New York,” Trepka said.
“The Miami-Dade Water and Sewer Department is investigating opportunities to add the monitoring of the polio virus to our wastewater surveillance program, where it makes sense, in the effort to continue the documentation of information for the benefit of the public health,” said Jennifer Messemer-Skold, public affairs administrator for the department.
What is polio?

Polio, or poliomyelitis, is a disabling and life-threatening disease caused by the poliovirus. The polio virus spreads from person to person and can infect a person’s spinal cord, causing paralysis, according to the Centers for Disease Control and Prevention.
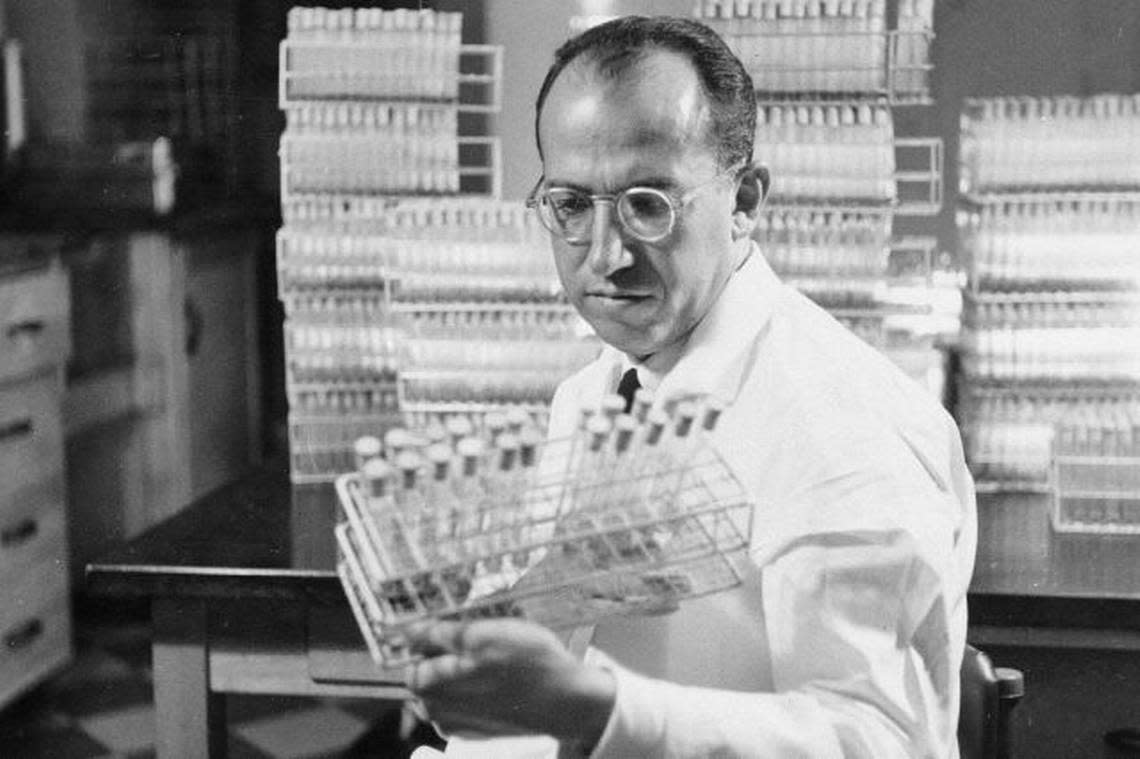
Polio was once a terror in the 1940s and ‘50s in the United States, Canada and elsewhere before virologist Jonas Salk’s polio vaccine was first administered in 1955. Some famous people who contracted polio before there was a vaccine include U.S. President Franklin Delano Roosevelt, musicians Joni Mitchell and Neil Young and actors Alan Alda, Mia Farrow and Donald Sutherland.
In the early 1950s, before Salk’s vaccine, polio outbreaks caused more than 15,000 cases of paralysis each year, the CDC said. After the vaccines — there are two: trivalent inactivated poliovirus vaccine (IPV), introduced in 1955, and trivalent oral poliovirus vaccine (OPV) in 1963 — the number of polio cases plummeted to fewer than 100 in the 1960s and fewer than 10 in the 1970s.
I thought polio was a devastating disease of the past. Unfortunately, it’s not | Opinion
How contagious is polio?
“Polio is transmitted person to person through the fecal oral route, by contact with stool from an infected person or by droplets such as after an infected person coughs,” Trepka said.
“For example, an infected person’s hands can get contaminated with stool after using the toilet and remain contaminated if there is poor hand washing. That person can then contaminate food that another person consumes and thus expose the person to the polio virus,” she said.
What are polio’s symptoms?
Symptoms can include sore throat, fever, fatigue, nausea, headache and stomach pain, according to the CDC. These symptoms mirror many other ailments. A healthcare provider can take swabs from the throat and collect stool samples to send to a lab for testing.
According to the CDC, a large majority of people who are infected with polio may have no symptoms, about 72%; about 25% have a flu-like illness. A small percentage, about one in 200, of individuals who contract the polio virus suffer paralysis. A few could contract meningitis if the polio virus attacks the covering of the spinal cord or brain. Polio is fatal for 2%-10% of those paralyzed or between 1 in 2,000 to 1 in 10,000 of those infected.
READ NEXT: ‘Florida is in midst of a meningococcal outbreak.’ What to know now about meningitis
Why are polio, monkeypox and meningitis reemerging?
“Monkeypox is a different issue from the situation with polio. Polio is a disease that we normally successfully prevent when we have high rates of children vaccinated,” Trepka explains.
READ NEXT: As monkeypox spreads in South Florida, experts have advice on prevention, risk, vaccines
“Small outbreaks of vaccine-preventable childhood diseases are not new because we do not have universally high rates of childhood vaccination. We continue to have outbreaks, albeit relatively small ones, of vaccine-preventable disease such as measles and pertussis. These happen whenever you get a pocket of people who are not fully vaccinated. It has been challenging to keep vaccination rates high,” she said.
Lack of first-hand experience can be a factor.
“One of my mother’s classmates died of polio while she was in middle school; thus, she had first-hand knowledge of the devastating consequences of polio and fully supported having her own children vaccinated. However, because of the success of the U.S. childhood vaccination program, few parents of young children have personally experienced the devastating consequences of previously common childhood diseases, such as measles, pertussis, polio and diphtheria, that we now prevent with vaccines. Thus, some people don’t understand the full benefit of these vaccines and how they have made childhood a much less dangerous time than it used to be,” Trepka said.
“At the same time, the internet has provided a forum for widely disseminating inaccurate information about vaccines. I think it is challenging for many people to differentiate accurate from inaccurate information. Thus, while vaccine hesitancy is not new, the challenge to keep childhood vaccination rates high is greater than it has been in the past,” Trepka said.
We’re facing a triple threat of COVID, monkeypox and polio. Let’s take them seriously.
Is there a vaccine for polio?

Polio remains one of the standard childhood vaccines.
Since 2000, only the inactivated polio vaccine (IPV) has been used in the United States, which is an injection, usually to the arm or leg, according to the CDC.
“The oral polio vaccine is not used in the U.S. because it is live attenuated vaccine, meaning that it exposes the body to a weakened version of the virus leading to an immune response and not infection in people with healthy immune systems. However, there is a risk of infection among people with weakened immune systems. The IPV does not have this risk,” Trepka explained.
The IPV vaccine is four doses -- at 2 months of age, 4 months, 6-18 months and 4-6 years.
I’ve never been vaccinated for polio. Should I now?
Yes. People who have never been vaccinated for polio should definitely get vaccinated regardless of their age, Trepka said. For adults who have never been vaccinated, three doses are needed with the second dose one to two months after the first and the third dose six to 12 months after the second, according to the CDC.
I was vaccinated for polio. Do I need a booster?
“At this point, there is not a recommendation for a booster for the general population,” Trepka said. “However, there is a one-time lifetime booster recommendation for a select group of people, namely travelers to a country where there is a high risk of polio, laboratory workers or healthcare workers who may handle specimens with polio, or for people who have been in close contact with a person with polio virus.”
“There has been a global effort to eliminate polio for many years. Unfortunately, it has been unsuccessful because unlike smallpox, which we did eradicate, a high percentage of people infected with polio have no symptoms. Also the problem of vaccine hesitancy is a global one and has thwarted polio eradication in some countries. Until polio is eradicated from the world, we will need to continue childhood vaccination for polio in the United States,” Trepka said.
How do you know if you’ve been vaccinated?
Florida SHOTS is Florida’s immunization registry, which began in 2003. All children born in the state beginning in 2003 have been automatically added to the system unless the parent of the child made a special opt out request. It includes information about vaccines administered by the Florida Department of Health as well as health care providers in Florida who use the system. It includes recent vaccines for adults to such as COVID-19 vaccines.
You can ask your healthcare provider to search the Florida SHOTS database for you. If you are 18 and older you can also submit a request to obtain your vaccination records from Florida SHOTS by filling out an online form.
If you’re a parent you know whether your children are vaccinated.
But what if you are older, say, in your 50s or older, and can’t find your pediatric vaccination records or have no one in your immediate family to ask whether you received the polio vaccine decades ago.
If you are this person and went to school in Florida or anywhere else in the U.S. or Canada or countries where having the polio vaccine was mandatory to attend school, you’re good. You’re vaccinated, assured Dr. Jenny Montes de Oca at Coral Gables’ Prime Care Associates to one of her 59-year-old patients who went to grade school in Miami Beach in the late 1960s and 1970s.
You can also try to contact the health department in the place in which you were born.
“Immunization registries are relatively new. Thus, for many adults, we can only know if we were vaccinated as children if our parents gave us the paper records or if a parent actually recalls the vaccine administration and recall can be unreliable. The current children of Florida won’t have that problem when they are adults since their records are in one place and will be accessible to them,” Trepka said.
For travelers
How do you know if you are traveling to a country with a high risk of polio and whether you ought to consider a polio booster?
The Centers for Disease Control and Prevention has an International Traveler’s Health Website where you can look up specific recommendations for the countries you are traveling to. The information is continually updated based on epidemiologic information from around the world.
“Currently, there are many countries in Africa as well as the countries Afghanistan, Israel, the Occupied Palestinian Territories, Pakistan, Ukraine and Yemen, which are considered high risk for polio, and thus polio booster doses are recommended for those who have not previously had a booster,” Trepka said.
