Paxlovid helps prevent severe illness from COVID. Why don't more people take it?
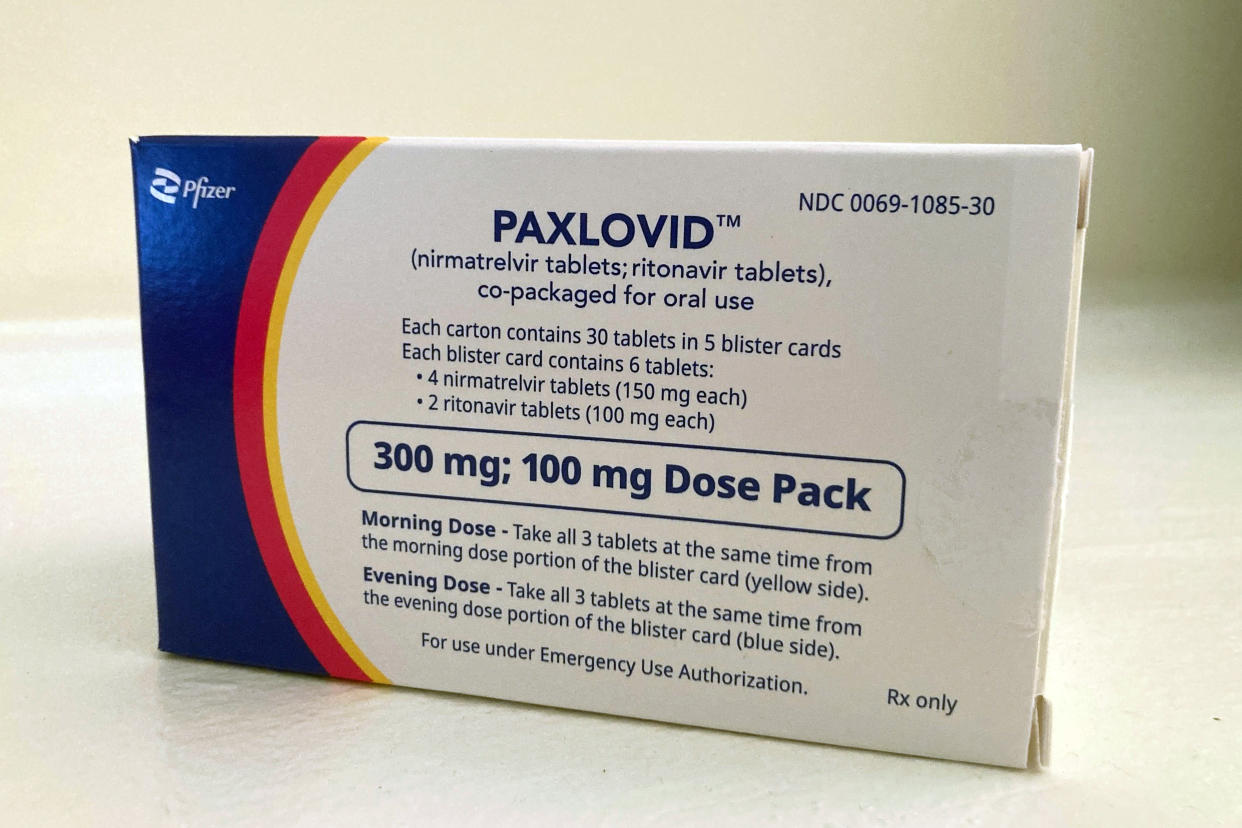
With the current COVID-19 death toll in the U.S. at more than 1.1 million and new evidence that COVID infections can damage the brain, heart and lungs, it's clear that the disease is more than “just a bad cold.” Paxlovid, which is a combination of two drugs (nirmatrelvir and ritonavir), can lower the risk of severe symptoms and reduce hospitalizations. But not enough people are offered the drug when they test positive. A recent study by the National Institutes of Health found that only 15% of people who were eligible for the drug took it. Here's what you need to know about Paxlovid, including who should take it and when.
How does Paxlovid work?
Paxlovid is an antiviral therapy that helps your body fight off COVID-19 faster and more effectively. In one clinical trial, Paxlovid was 89% effective in reducing hospitalization and death in patients who were not vaccinated and were at risk for severe disease.
“Paxlovid is made up of two separate medications — nirmatrelvir and ritonavir — both in pill form,” Dr. Alexander Fortenko, an emergency medicine physician with Weill Cornell Medicine, tells Yahoo Life. “Nirmatrelvir is a drug that inhibits the production of an enzyme that the COVID-19 virus needs to reproduce. The other pill, ritonavir, slows down how quickly nirmatrelvir is broken down by the liver, essentially providing a boost for it.”
When should you take Paxlovid? Is there anyone who shouldn't take it?
Timing matters when it comes to taking Paxlovid. “Nirmatrelvir/ritonavir has to be started within the first five days of symptoms, and it has to be prescribed by a doctor,” Dr. Linda Yancey, director of infection prevention at the Memorial Hermann Health System in Houston, tells Yahoo Life. “If you would like to take the medication, call your health care provider right away, as soon as you feel sick and test positive for COVID-19.” The course involves taking three pills twice a day for five days, and patients need to finish the prescription even if they feel better.
“Paxlovid is for the treatment of adult and pediatric patients — 12 years of age and older weighing at least 88 pounds — with mild to moderate COVID-19 and who are at high risk for getting severe COVID-19, including hospitalization or death,” Hai Tran, a clinical pharmacist and director of Drug Use Policy at Cedars-Sinai Medical Center in Los Angeles, tells Yahoo Life.
According to the CDC, people with a high risk of severe disease include older adults, people with other health conditions such as obesity, diabetes and cancer, people with disabilities and certain racial minorities.
However, not everyone can take Paxlovid. It’s not recommended for people with a low risk of severe disease, and it should not be taken by people with allergies to any of its ingredients, people on certain medications such as statins and Viagra, people who are pregnant or breastfeeding and those with liver or kidney disease.
Why do some doctors not prescribe it?
While there hasn’t been definitive research on why some doctors don’t prescribe Paxlovid, the reasons may include initial shortages of the drug countrywide, doctors not being familiar with the drug and people often coming to doctors after the five-day prescription window had passed. There are also concerns about drug-to-drug interactions in people who are on other medications, such as statins.
“Doctors may not all be familiar with the data about how much of a difference Paxlovid can make in the right patient population,” says Fortenko. “They may also not be aware of how to augment or adjust the patients' standard medications to make Paxlovid a safe, viable option.”
What are the side effects of Paxlovid?
Paxlovid has relatively few side effects — the most common being temporary nausea, altered taste and diarrhea. Other side effects to watch out for are abdominal pain, increased blood pressure, muscle aches and feeling unwell. Also, it’s important to look out for signs you may be allergic to any components of the medication, such as hives, skin rash, difficulty breathing, tightness in the throat and swelling of the mouth, lips or face.
Some patients have reported experiencing rebounds, also known as COVID rebounds or Paxlovid rebounds, which is when COVID-19 symptoms reoccur in people after they have gotten better. However, research shows that rebounds are not more common after taking Paxlovid than they are in people who didn’t take the medication. They’re now thought to be a normal part of the COVID-19 infection process in some people. A CDC study found that rebounds happened in less than 1% of people who took Paxlovid.
“The rebound effect is not unique in people who take Paxlovid,” says Tran. “And there is no increase in the risk of death or hospitalization if you have a rebound. Also, you don’t need to take more Paxlovid for it.”
Does Paxlovid help prevent long COVID?
There’s conflicting evidence on the effect Paxlovid has on long COVID, also known as post-COVID condition. One study found that Paxlovid reduced the risk of long COVID in all participants regardless of vaccination or number of previous infections. However, another more recent study found that Paxlovid does not reduce the risk. Since Paxlovid is still a relatively new drug and the COVID-19 virus is still changing, it may take some time for a definite answer to emerge.
Should you get Paxlovid if you test positive for COVID-19?
If you test positive for COVID-19, it’s a good idea to ask your health care provider as soon as possible if taking Paxlovid would be helpful for you. As a reminder, you’ll need to do this within the first five days of symptoms to be considered. And you would need to meet all the criteria before you are placed on the drug.
It’s also important to follow the prescription’s instructions. This means continuing the drug even if you feel better. Also, Paxlovid should not be used to try to prevent COVID-19 infections — it’s meant for people who test positive and are at high risk of severe disease and who also meet other prescription criteria.
“The best way to treat COVID-19 is to never catch it at all,” says Yancey. Preventive measures such as handwashing, masking and up-to-date vaccines continue to be important in preventing the spread of the virus. But if these fail, and you test positive, Paxlovid may help you avoid severe illness and get better sooner.
Nsisong Asanga is a writer, public health physician and field epidemiologist.
