Ovulation Pain and Relief Options
Medically reviewed by Renita White, MD
Ovulation is when the ovary releases an egg. It is part of the menstrual cycle for most people with a uterus. Some people experience ovulation discomfort, known as "mittelschmerz," which is German for "middle pain."
Ovulation pain involves pain or cramps on one side of the lower abdomen, pelvis, or lower back. It may alternate between the left and right sides between menstrual cycles, but the discomfort remains on one side throughout that ovulation cycle.
This article reviews why ovulation causes pain and the location, sensation, and timing of ovulation pain. It also covers other ovulation symptoms and when to discuss it with a healthcare provider.
The Ovaries and Ovulation
The ovaries are small organs in the pelvis on either side of the uterus. They are about the size of an almond. Every month, the ovaries create tiny sacs called follicles, which hold immature eggs. If an egg combines male sperm during unprotected sex, it can result in pregnancy.
Ovulation usually happens in the middle of your menstrual cycle, roughly two weeks before your next period.
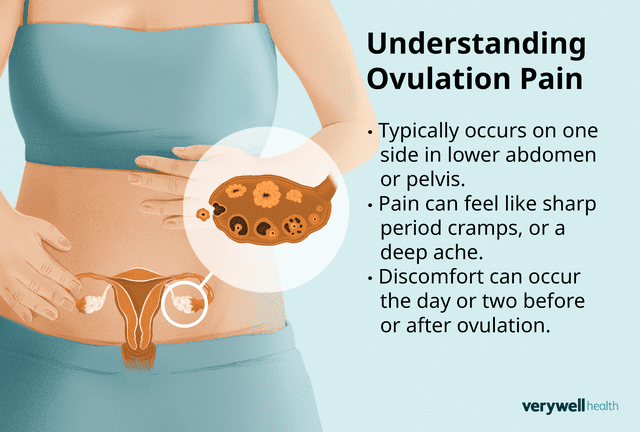
Illustration by Julie Bang for Verywell Health
Why Ovulation Causes Pain
Ovulation pain occurs because the ovary's wall stretches when the follicle breaks to release the egg. When the follicle breaks, it sometimes releases fluid or blood, irritating the abdominal lining. Intense pain may result from forceful follicle rupture. Fallopian tube (tube from the ovaries to the uterus) spasms can also cause discomfort.
Ongoing or intense pain may indicate underlying medical conditions. For example, endometriosis is a common gynecologic condition that can intensify ovulation and period pain. It occurs when tissue similar to the uterine lining grows outside the uterus. The tissue reacts to hormonal changes, causing bleeding and pain.
While this is not an exhaustive list, other conditions that can contribute to ovulation pain include:
Adenomyosis: Uterine lining grows into the uterine muscle
Adhesions: Scar tissue from previous surgeries or infections
Appendicitis: Appendix (small organ in the lower right belly) swelling
Ectopic pregnancy: Fertilized egg implants outside the uterus
Fibroids: Noncancerous growths in the uterus
Ovarian cysts: Fluid-filled sacs on the ovaries that can rupture
Ovarian hyperstimulation syndrome: Complication of fertility treatments
Ovarian torsion: Twisting of the ovary
Ovarian vein thrombosis (rare): Blood clot in the ovarian vein
Pelvic inflammatory disease (PID): Infection of the female reproductive organs
Polycystic ovary syndrome (PCOS): A hormonal condition that causes the ovaries to get large and develop cysts
Urinary conditions: This includes urinary tract infections (UTIs), kidney stones, or interstitial cystitis (IC, chronic bladder inflammation)
Related: Pelvic Pain
Does Ovulation Pain Get Worse Around Menopause?
Perimenopause, the time leading up to menopause, causes fluctuating hormone levels. These fluctuations can worsen ovulation pain and menstrual cramping. However, once you enter menopause (not having a period for 12 consecutive months), you should not ovulate or have ovulation pain.
Related: Perimenopause Treatment and Self-Care Ideas
Pinpointing Ovulation Pain
While not everyone experiences ovulation pain, those who do can use their symptoms to glean insights into the timing of ovulation and aid in family planning.
Location
Ovulation pain typically stays in one area, on one side of the lower abdomen or pelvis.
The location is likely on the side where the ovary releases the egg. It can alternate sides each menstrual cycle or stay on the same side for several months in a row. But it will remain on the same side throughout ovulation. Some people also feel it in their lower back.
Sensation
Ovulation pain descriptions include sharp period cramps, a twinge, stabbing pain, or deep aching. Sometimes, it comes and goes, but it can also be a constant or nagging sensation. People note that it is different from other types of pain.
Additional Ovulation Symptoms
Hormonal changes can also cause other ovulation symptoms like:
A slight increase in basal body temperature, about 0.5 to 1 degree F
Bloating
Breast tenderness
Increased sex drive
More abundant, clear, thin, slippery, and stretchy vaginal discharge
Timing in Cycle
Ovulation occurs about midway through the menstrual cycle, typically about 14 days before starting your next period. Discomfort can occur the day or two before or after ovulation.
Duration Of Pain
The duration of ovulation pain can also vary, lasting anywhere from a few minutes or hours up to 48 hours.
When to Discuss Ovulation Pain With a Provider
While mild discomfort during ovulation is expected, if you experience severe or persistent pain, consult a healthcare provider to determine the underlying cause and the appropriate treatment, especially for any of the following symptoms:
The type or severity of ovulation pain changes
Pain that lasts longer than usual (more than 48 hours)
Painful urination (peeing) or bowel movements (pooping)
Atypical vaginal bleeding (other than light spotting) with ovulation
Pain with sexual intercourse
Vomiting or diarrhea with ovulation pain
The pain does not go away with home care (like a warm bath or over-the-counter pain relievers)
Treatment and Relief for Pain During Ovulation
Most of the time, ovulation pain is mild and resolves independently. Sometimes, a warm bath or heat therapy can help. If these methods don’t work, consider over-the-counter (OTC) pain relievers, including:
Advil, Motrin (ibuprofen)
Aleve (naproxen)
Tylenol (acetaminophen)
How to Manage Monthly Ovulation Pain
You might find that starting pain relievers a day or two before you anticipate ovulation or as soon as you begin to feel a twinge of pain helps you better manage monthly pain. Waiting until the pain level is high can make it more difficult to control. Check with a healthcare provider to ensure this is a safe approach.
If you have endometriosis that causes severe ovulation pain or cramps, you can try complementary and supportive therapies like massage, chiropractic care, acupuncture, or herbal remedies. Herbal pain relief options include:
Cannabis, namely strains high in cannabidiol (CBD) and low in tetrahydrocannabinol (THC)
Ginger
A healthcare provider may also suggest prescription anti-inflammatory pain medications such as Ponstel (mefenamic acid) or Celebrex (celecoxib), muscle relaxers like Valium (diazepam), nerve blocks, physical therapy, or surgery.
Can Birth Control Help?
Hormonal contraceptives can help you manage ovulation pain by preventing ovulation or regulating hormone fluctuations. Combination birth control pills, containing estrogen and progestin, make your brain think ovulation has already taken place.
It’s essential to take birth control pills at the same time every day. If you miss more than one pill in a row, there might not be enough hormones in your body to trick your brain, causing you to ovulate.
Hormone Therapy for Endometriosis
If you have endometriosis, your provider may also suggest different hormone therapies like gonadotropin-releasing hormone agonists (GnRH) or aromatase inhibitors.
Summary
Ovulation pain occurs on the left or right side of the lower abdomen, pelvis, or lower back. It may feel like sharp period cramps, a twinge, stabbing pain, or deep aching that comes and goes or remains constant. Ovulation discomfort occurs in the middle of your menstrual cycle when the ovaries release an egg.
Management strategies include heat, over-the-counter pain relievers, complementary therapies, and, in severe cases, consulting a healthcare provider.
Read the original article on Verywell Health.
