How to overcome COVID-19 going forward

Where exactly do we stand with the pandemic right now?
A few months ago when vaccination rates were accelerating and COVID-19 cases were plummeting, it seemed we were out of the woods. Offices, colleges and universities, sports leagues, resorts and concert halls were making plans to fully reopen, yes with restrictions, but net-net it looked like the pandemic was winding down and we’d have a pretty normal fall.
Not so fast.
Now we’re seeing vaccinations plateau, the Delta variant rear its ugly head and breakthrough cases come to the fore. The reopening process has stalled or has been thrown in reverse. Confusion and frustration are returning.
On Wednesday for instance, the 121-year-old New York Auto Show, which was to be held from Aug. 20-29, was nixed, after being postponed earlier this year. Here’s the statement:
“It is with great disappointment that the upcoming 2021 New York International Automobile Show at the Jacob K. Javits Convention Center has been cancelled due to the growing incidences of the COVID-19 Delta variant and the increased measures announced recently by state and local officials to stop its spread.”
The show’s management expected 1 million visitors with exhibits from 34 carmakers and more than 100 other vendors. Planned introductions reportedly included the 2022 Jeep Grand Cherokee, Nissan Z, and Subaru WRX.
Consider the economic impact. And that’s just one event. Think of the thousands of wedding planners, school administrators and restaurant owners (never mind the folks who run hospitals and urgent care facilities) trying to make their way through all this.
Yes, Friday’s jobs report for July was strong, (some call them "pre-Delta" numbers), but caution signals are beginning to flash. IHS Markit recently downwardly revised its global GDP growth forecast to 5.8% in 2021, noting that “global economic growth depends increasingly on COVID-19 vaccination progress.”
On Thursday, Amazon and Wells Fargo announced they were delaying their return to work schedules (and they are not alone) because of uncertainty surrounding COVID-19.
Another indicator, the yield on the 10-year Treasury bond that climbed smartly since last fall signaling a pick-up in economic activity, peaked at the end of March. It has since fallen from 1.7% to a low of 1.1%, reflecting investors' newfound fear of a slowdown.
In a sense then, we’re back to square one with COVID-19, once again trying to discern the indiscernible — the course of a pandemic. The implications couldn't be larger.
Which brings me back to my opening question: Where are we exactly? Not the beginning clearly, but are we near the end, or is it really more like the middle?
To help figure that out, I decided to go back and look at the trajectory of previous pandemics for clues. For sure, there are limitations to that kind of inquiry as much of this is (literally) ancient history. Still, it turns out there’s actually some pretty interesting stuff to noodle over.
Obviously the most useful parallel is the Spanish (more on that word in a second) flu pandemic of 1918-1920. And there, right away that jumps out at you ... all those years. Does that inform us in any way?
Perhaps a bit.
'Nobody knows'
First, let’s pinpoint exactly when the COVID-19 pandemic began. Obviously in 2019, ergo the name, but remember it was the last month of the year. Here is the salient line from an article in The Lancet:
"In late December 2019, an outbreak of a mysterious pneumonia characterized by fever, dry cough, and fatigue, and occasional gastrointestinal symptoms happened in a seafood wholesale wet market, the Huanan Seafood Wholesale Market, in Wuhan, Hubei, China."
(The exact origins of the disease, whether it was zoonotic — i.e., jumping species — or lab leak, are of course a matter of debate. You might not have seen that former President Donald Trump recently suggested that China pay the U.S. reparations for COVID-19 and “$10 trillion, that wouldn't cover it.”)
So, let’s just say for measuring purposes then that the COVID-19 pandemic began on Jan. 1, 2020. Therefore, the COVID-19 pandemic is some 19 months old. Does that mean we’re halfway?
Who better to put that question to than one of the National Institutes of Health’s 1918 flu experts, Dr. David M. Morens, senior adviser to the director of the National Institute of Allergy and Infectious Diseases. In 2007, Morens co-authored “The 1918 Influenza Pandemic: Insights for the 21st Century" with none other than Dr. Anthony Fauci.
How much can we look to 1918, I ask? Turns out not that much.
“If you look back at the news reports over the last year-and-a-half, you see that everybody and their brother's making predictions about what's going to happen, but nobody knows,” Morens says. “And most of the predictions are wrong, because we don't have anything to compare it to. Influenza doesn't provide us a very good template to figure out what's happening with SARS-CoV-2 [the virus that causes COVID-19.]"
Why is that?
To borrow a phrase from "Anna Karenina:" Pandemics are like unhappy families; each one is problematic in its own way.
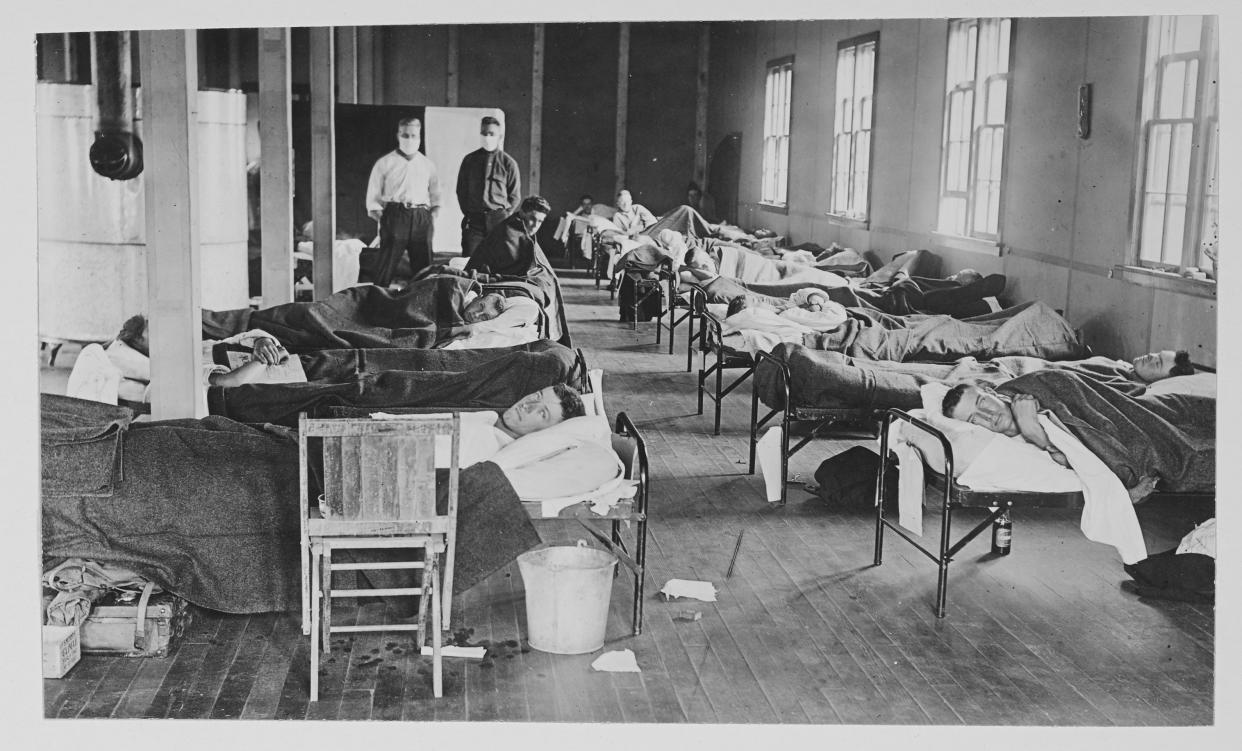
The 1918 pandemic was different from this one in two broad ways. First, the 1918 virus itself acted very differently (it tended to arrive and leave a community in a much more intense fashion). And second, the times were different. It occurred during a World War and before viral vaccines.
Let’s first drill down into the two viruses.
“The flu and SARS-CoV-2 are both made from RNA, but they're completely different,” Morens says. “They're as different as a man and a mouse. As different as apples and oranges.” NB: When I asked Morens which one was worse, he picked the influenza of 1918 because it was much more lethal.
The specific biological distinction — spelled out in this excellent article in The Conversation from 2020, (written by two University of Pittsburgh PhDs) — are pretty technical, but I will tell you that those differences have several implications. For one thing, as this research paper notes, “Victims of the 1918 influenza mostly died from secondary bacterial pneumonia, while victims of COVID-19 mostly died from an overactive immune response resulting in organ failure.”
Another important distinction from The Conversation article is that the influenza virus was much better at mutating, which was bad of course, except that it led to more predictable and seasonal waves of the disease. The virus that causes COVID-19 is actually more stable, which should mean that “physical distancing and mask-wearing will keep its spread in check and, ideally, keep infection and death rates steady,” according to the article.
But it also means that “as states loosen non-pharmaceutical interventions, the U.S. will likely experience a long plateau of continued new infections at a steady rate, punctuated by periodic local flares,” the article added.
The authors suggest that outbreaks of COVID will be driven not so much by mutations — Delta variant notwithstanding — but by exposure of non-immune (mostly unvaccinated) people to the virus. And here’s the money line: “Future spikes in COVID-19 cases and deaths will very likely be driven by what people do.” (Emphasis mine.) In other words, if we don’t get vaccinated and change social behavior when needed, the disease will stay with us.
Another critical distinction between COVID-19 and the 1918 influenza or Spanish flu pandemic, as noted previously, is historical context. The first case of the influenza pandemic is generally considered to have been in Kansas in March 1918. (Scientists aren’t sure why.) The disease came and went in those aforementioned waves, pretty much petering out after wave number four in the spring of 1920, or after almost exactly two years.
An estimated 500 million, or about a third of the world’s population, were infected, with some 25 million to 50 million deaths, (more than the 20 million who died in World War I), including some 675,000 deaths in the U.S. That’s just a bit more than the current 615,000 U.S. deaths from COVID-19, but the U.S. population in 1918 was around 103 million, versus 328 million today. Those 675,000 deaths back then would be the equivalent of 2.1 million deaths today.
You may not be surprised to learn that "Spanish flu" is a misnomer, as Wikipedia explains: “To maintain morale, [World War I] censors suppressed bad news in the belligerent countries, but newspapers were free to report the epidemic's effects in neutral Spain, including the grave illness of King Alfonso XIII. These stories created a false impression of Spain as especially hard hit, leading press outside Spain to adopt the name "Spanish flu.”
(BTW, the Spanish called it the French flu and the French called it the American flu, but changed to Spanish so as not to upset a war ally. And of course French fries are called "pommes frites" in France, but that’s another story.”)
Speaking of World War I, that conflict greatly exacerbated the effects and impact of the influenza pandemic. Overcrowding in troop camps, ships and POW prisons, movements of large armies around the globe as well as poor health conditions and nutrition probably all increased transmission, augmented mutation and reduced people's resistance to the virus.
Just like today, some folks back in 1918 and 1919 resisted wearing masks. And also just like today, some politicians figured it out and some didn’t. In 2018, on the 100th anniversary of the influenza pandemic, my pal Shelley Hearne, then president of CityHealth and now director of Johns Hopkins Center for Public Health Advocacy, wrote about how two cities, Philadelphia and St. Louis, reacted to the influenza pandemic with radically different consequences (Philly did nothing and thousands died, while St. Louis — then one of the 10 largest cities in the U.S. — locked down and experienced one of the lowest excess death rates in the nation.) Hearne, presciently, urged us to take heed.
'Not like flipping a light switch'
Back in March, I asked Dr. Francis Collins, director of the National Institutes of Health, (and Tony Fauci’s boss), about when we will be back to normal.
“Well, define normal, Andy, because I don't think we'll ever go back to quite the way we were before this, in some fairly trivial ways,” he says. “So for instance, as NIH director, I used to spend an awful lot of time taking very long trips to meetings where I might speak for 45 minutes and then get back on a plane and go home again. You can do this kind of thing pretty effectively using Zoom and other measures."
Bottom line, Dr. Collins, please. When is normal?
“So it's going to happen gradually,” Collins told me. “It's not like flipping a light switch. It's going to be bit by bit.”
Morens offered a more sobering perspective. “This virus looks like it will never go away,” he says. “So we're stuck with it forever, probably. And eventually people will get immune by being affected, or by being vaccinated. And that would hopefully make the virus circulate at a much lower level and kill fewer people. But the scenario that we had with 1918, where the virus becomes seasonal and we only get it in the winter and then it's wimpy most years, but some years it's worse than others, we just don't know if that's going to happen. And for a year and a half, there's no evidence that it will happen, but that doesn't mean it won't."
“The viruses are moving targets that are evolving at a very rapid rate,” Morens says. “And whatever is true today, probably is not going to be true six months from now. The least you can say is these vaccines protect people long enough to buy time, to make better vaccines, or perhaps in the future give additional doses of the vaccines.”
It sounds trying and difficult, and it is. But we can manage this thing. Overcome it. We just need to be vigilant.
The key takeaway to me is this. Between our understanding of this new virus and our game-changing vaccines, we can control our own destiny in a way we couldn’t 100 years ago. Right now, though, not enough of us comply with mask mandates and are willing to get vaccinated. I keep going back to that line in The Conversation article: “Future spikes in COVID-19 cases and deaths will very likely be driven by what people do.”
That means us.
This article was featured in a Saturday edition of the Morning Brief on August 7, 2021. Get the Morning Brief sent directly to your inbox every Monday to Friday by 6:30 a.m. ET. Subscribe
Andy Serwer is editor-in-chief of Yahoo Finance. Follow him on Twitter: @serwer. Ben Werschkul is a writer and producer for Yahoo Finance in Washington, DC.
