9 things Texans need to know about monkeypox — from transmission to vaccination
Monkeypox is spreading in Texas.
In early June, Dallas County reported the state’s first case of the monkeypox virus infection this year. The patient, who had traveled internationally the past month, isolated at home, according to a press release from the Texas Department of State Health Services.
Monkeypox is a rare viral disease transmitted to humans through close contact with an infected person or animal. It can also be transmitted from person to person by inhaling large respiratory droplets or through close contact with body fluids and lesions, as well as bedding and other contaminated materials. Those infected may experience fever, rash and swollen lymph nodes, as well as more serious complications, per the Texas Department of State Health Services.
These are nine things you should know about the state of monkeypox in Texas.
1. Most cases are in North Texas
There are 183 cases reported across Texas, with the most cases, 89, in North Texas, according to the health department. The second most cases (51) are in the Houston area and the third most are in Central Texas, with 36 cases. There are also six cases in the San Antonio region and one in the Texas Panhandle.
DSHS told the Star-Telegram that most cases have been transmitted by direct skin-to-skin contact, generally through sexual or other intimate contact. The early cases were related to international travel. As of last week, about 10% of patients report having traveled internationally, with 25% each saying they had traveled domestically or not at all. Travel is unknown for the remaining 40%.
Overall, 2,891 cases have been confirmed in the U.S., with the most cases in New York and California. Throughout the world, 16,836 cases have been confirmed in 74 countries.
2. Males and young adults are getting it the most
Most, or 180 monkeypox cases, were male patients. Only three females in Texas have gotten the illness.
Texans in their thirties are the biggest age group with the illness, making up 76 reported monkeypox cases. Young adults, from 18 to 29 years old, made up the second largest group, with 58 cases in the state. Thirty-one adults in their forties had monkeypox in Texas, as well as 16 in their fifties, and two over 60 years old.
3. You can get it through close contact
Anyone who has been in close contact with someone who has monkeypox is at risk, the CDC says.
Monkeypox can spread when a person comes into contact with the virus from an infected animal, infected person, or materials contaminated with the virus, per the CDC. The virus can also cross the placenta from the mother to her fetus.
Monkeypox spreads between people primarily through direct contact with infectious sores, scabs, or body fluids, or with materials that have touched body fluids or lesions, such as clothing or linens. Monkeypox can spread during sex, as well as activities like kissing, cuddling, or touching parts of the body with monkeypox sores. It also can be spread by respiratory secretions during prolonged, face-to-face contact.
4. You can get monkeypox from animals
The virus may spread from animals to people through the bite or scratch of an infected animal, by handling wild game, or through the use of products made from infected animals. It is not yet known what animal maintains the virus in nature, although African rodents are suspected to play a part in monkeypox transmission to people, according to the CDC.
There are several measures that can be taken to prevent infection with monkeypox virus, according to the CDC:
Avoid contact with people who have a new or unknown rash, lesions, or scabs.
Avoid contact with animals that could harbor the virus, including animals that are sick or that have been found dead in areas where monkeypox occurs.
Avoid contact with any materials, such as bedding, that have been in contact with a sick animal.
Isolate infected patients from others who could be at risk for infection.
Practice good hand hygiene after contact with infected animals or humans. For example, wash your hands with soap and water or use an alcohol-based hand sanitizer.
Use personal protective equipment when caring for patients.
5. It can take up to two weeks for symptoms to appear
The time from infection to symptoms for monkeypox is usually seven to 14 days but can range from five to 21 days. The fever precedes the rash by a couple of days, so you’ll notice a fever first, according to Dr. Nikhil Bhayani, Texas Health infection prevention and epidemiology physician advisor.
6. Monkeypox is milder than smallpox
The symptoms of monkeypox are similar to but milder than the symptoms of smallpox, according to the CDC. Monkeypox begins with fever, headache, muscle aches, and exhaustion. The main difference between symptoms of smallpox and monkeypox is that monkeypox causes lymph nodes to swell while smallpox does not.
“Overall, it’s a mild self-resolving illness,” Bhayani says. “People who have compromised immune systems or they’re requiring agents to treat like rheumatoid arthritis or autoimmune conditions, folks with cancer, advanced HIV or advanced age, they’re at risk for severe disease.”
The illness begins with:
Fever
Headache
Muscle aches
Backache
Swollen lymph nodes
Chills
Exhaustion
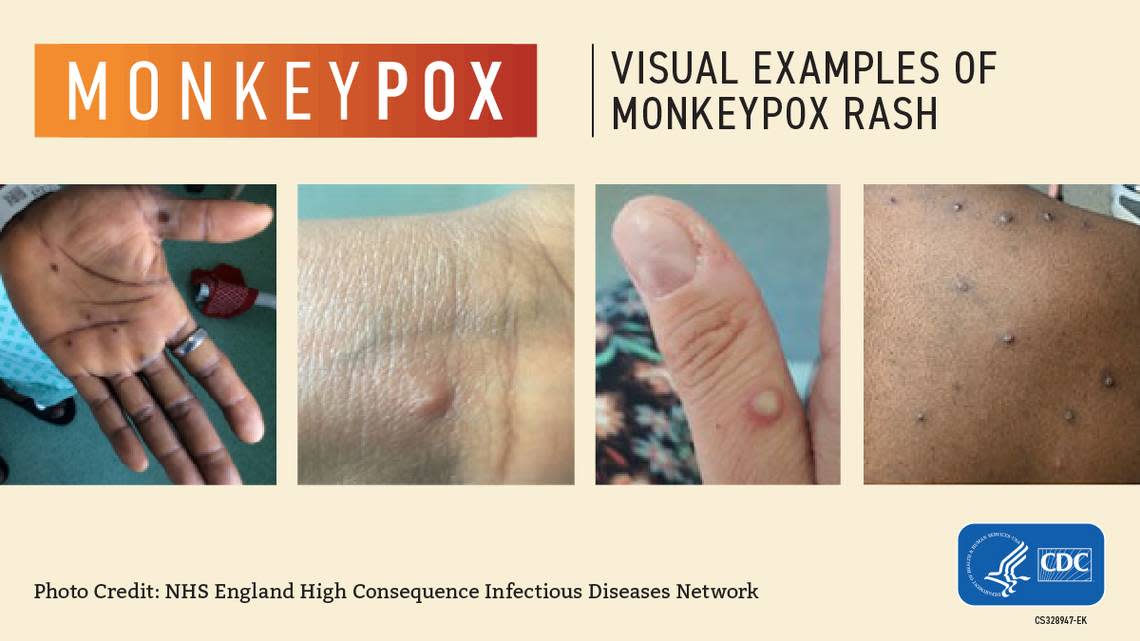
Within one to three days after the appearance of fever, the patient develops a rash, often beginning on the face then spreading to other parts of the body.
Lesions progress through the following stages before falling off:
Macules
Papules
Vesicles
Pustules
Scabs
The illness typically lasts for two to four weeks. In Africa, monkeypox has been shown to cause death in as many as one in 10 who contract the disease.
7. The risk to Texans is minimal
“Definitely there is a risk, but not to create enough panic,” Bhayani told the Star-Telegram. “There is a small risk, it’s just that we have to be aware that this virus is out there and it’s in various communities around the country and the world.”
DSHS spokesperson Anton also says the risk to the general public is currently low.
“People should be aware of the symptoms and seek medical treatment if they develop a rash, especially if they had contact with someone who had a rash that looks like monkeypox or after traveling to a place with recently confirmed cases of monkeypox,” Anton said.
In Tarrant County, suspected or confirmed monkeypox cases should be reported to the Tarrant County Public Health Department’s epidemiology division by calling 817-321-5350 or faxing a report to 817-850-2366.
8. Your doctor is probably monitoring patients for it
Texas doctors are on the lookout for the illness.
“DSHS issued a health alert for clinicians with information about the disease and recommendations on testing and diagnosis,” DSHS press officer Lara Anton told the Star-Telegram.
The DSHS and the CDC are urging health care providers in Texas to be alert for patients with rash illnesses consistent with monkeypox. Public health officials are working with local health care providers so that they are prepared to recognize monkeypox and report suspected cases.
“Just the routine stuff, just identifying patients who have the symptoms, and also where they have traveled. And then it’s up to the clinician to decide, did they fit the criteria for monkeypox testing? Have they been exposed to somebody with monkeypox? The symptoms are not specific so that’s the kind of information that the clinician would have to gather,” Bhayani explained.
Health care providers looking for guidance on diagnosis of monkeypox can consult with their local or regional health department, DSHS says.
9. Antiviral therapy, vaccine available
Currently there is no specific treatment approved for monkeypox virus infections. However, several antivirals developed for use in patients with smallpox can be beneficial in treating monkeypox. Healthy individuals with a mild case of monkeypox don’t need specific therapy. Patients considered for treatment include those with severe disease, people at high risk for severe disease and those infected in an especially dangerous part of the body.
“Usually it is a self-resolving illness through supportive treatment, but those people who have severe disease, there is antiviral therapy available, and you would have to consult with your local health department and the CDC to determine if the patient is appropriate for antiviral therapy,” Bhayani said. “There are vaccines available, but right now those vaccines are limited to folks in laboratory settings that are handling high-level specimens and also to the military.”
JYNNEOS, also known as Imvamune or Imvanex, is a vaccine approved by the U.S. Food and Drug Administration to prevent monkeypox. The vaccine is used to protect certain people who are at risk for exposure to monkeypox, including research laboratory personnel, clinical laboratory personnel performing diagnostic testing for orthopoxviruses, designated response team members, and health care personnel.