How do you know if you have long COVID? 5 things you need to know
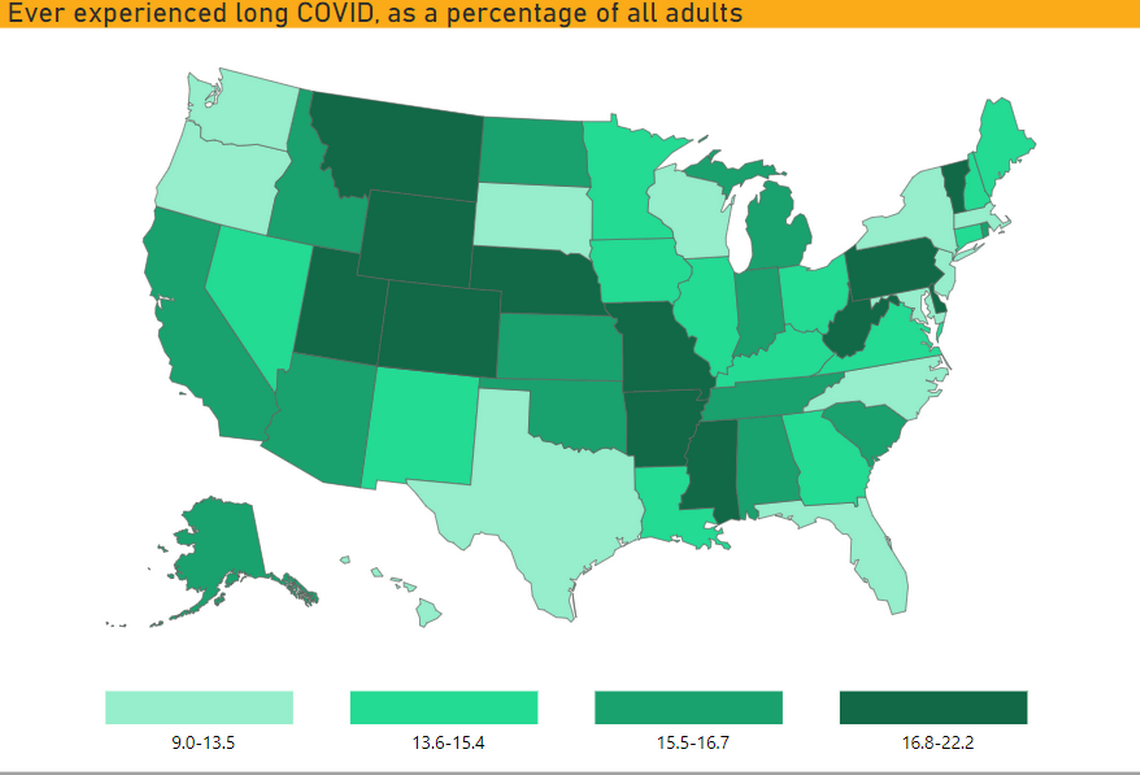
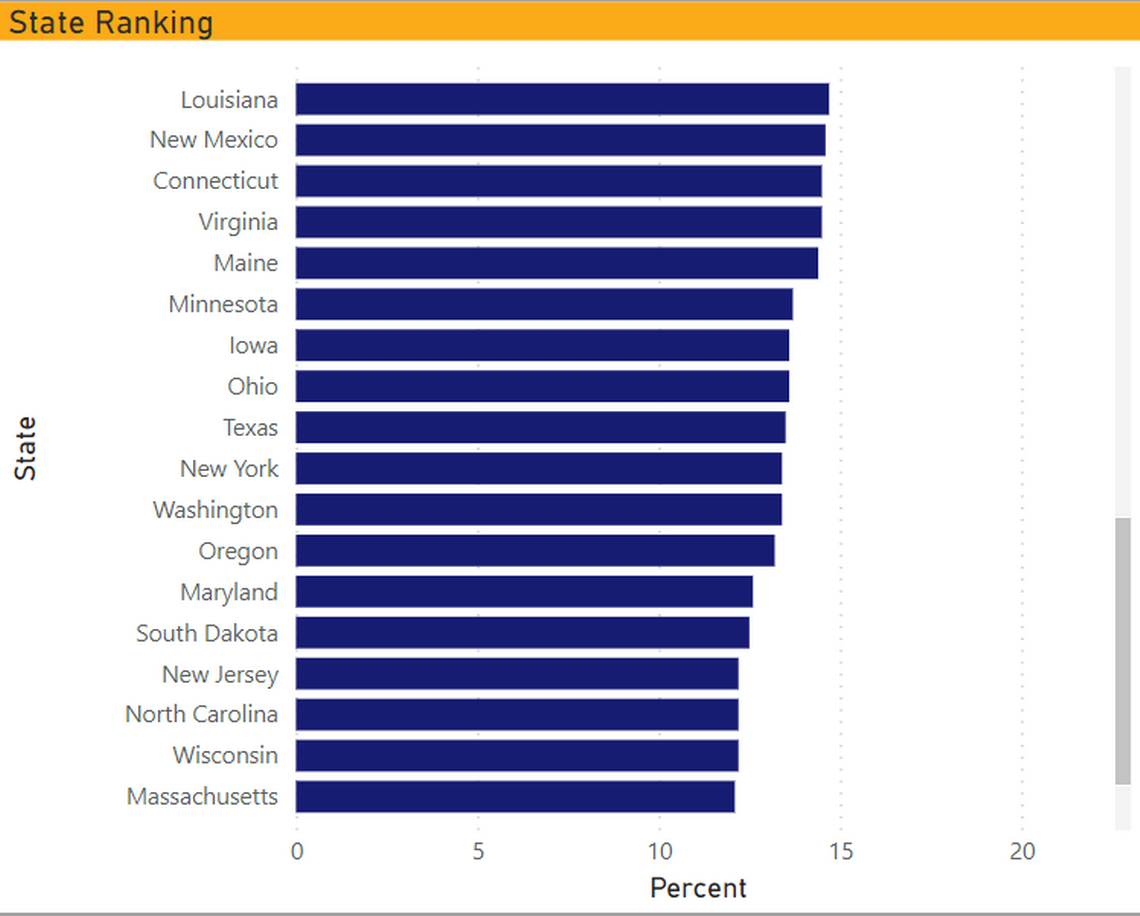
About 14% of Texans have experienced long COVID, according to a recent CDC survey, slightly lower than the national estimate of 15%.
Long COVID, also known as post-acute sequelae of COVID-19, is a syndrome in which people continue to experience symptoms of COVID-19 months after initial infection.
These are five things you should know about the state of long COVID in Texas.
1. A quarter of Texans who have had COVID have experienced long COVID
An estimated 26% of Texans who have had the virus have reported experiencing long COVID. That means they’ve had symptoms lasting three months or longer that they did not have prior to having COVID-19.
And 81% of Texas residents who have long COVID say that these long-term symptoms reduce their ability to carry out day-to-day activities. Worse, about 28% say there are “significant activity limitations.”
2. Several long COVID studies are being conducted in Texas
Because it is not a reportable condition, the Texas Department of State Health Services doesn’t track data on long COVID. However, several state universities are monitoring and treating the illness in Texas.
UT’s Post-COVID-19 Program provides medical care, research and education for patients who experience new or persistent symptoms months after their initial COVID infection. According to the UT program website, these include:
Fatigue
Deconditioning
Muscle weakness
Neuropathy and myopathy
Pain
Headaches
Exercise intolerance
Shortness of breath
Autonomic instability
Difficulty with thinking and concentration
Neurologic symptoms
Depression and anxiety
The care team includes internal medicine specialists, neurologists, advanced practice providers, nurses and social workers. They utilize the latest research, diagnostic and treatment techniques, allowing them to learn more about the emerging illness and develop diagnostic and therapeutic guidance as well as referral pathways to specialty providers.
The University of Texas Health Science Center at San Antonio is conducting the PREVAIL South Texas study (Prevention, Evaluation and Incidence of Long-Term COVID in South Texas) as part of the National Institutes of Health’s COVID research initiative. The study is looking into a drug that may help improve long COVID symptoms when taken nightly at bedtime for 14 weeks.
UT Southwestern has an outpatient rehabilitation program called COVID Recover, designed to help patients restore muscle, lung and brain function, mental health and psychological well-being after being infected with COVID-19.
The Inspire (Innovative Support For Patients with SARS-CoV-2 Infections) study at UT Southwestern aims to understand the long-term effects of COVID-19 infection. Participants describe how they are feeling by completing online surveys and share their medical information through a personal health platform.
3. Long COVID is more common in people who experienced severe symptoms requiring hospitalization
Serious symptoms that require hospitalization include severe inflammation, shortness of breath, confusion, persistent pain or pressure in the chest and organ damage, according to UT Southwestern.
The UT team’s research has found that one third of patients who were hospitalized and needed oxygen, and two thirds of patients who were hospitalized and needed a ventilator, have some level of lung scarring and tissue damage, making it hard for them to breathe. For patients who had the virus but didn’t need to be hospitalized, concerns include persistent cough, shortness of breath and respiratory issues.
However, anyone can experience long COVID, including young adults, healthy individuals and people who experienced mild COVID symptoms or were asymptomatic.
Risk factors, according to UT Health Austin, include:
Older age
Number of symptoms
Higher BMI
Females
History of asthma
4. People with long COVID experience a wide variety of symptoms
Symptoms of long COVID vary from person to person, per the UT long COVID website.
The most common symptom is chronic fatigue, which includes exhaustion, tiring with exertion and brain fog (difficulties with memory, lack of concentration, headaches, confusion and decreased mental clarity). Long COVID can also cause more serious health conditions including heart damage, lung damage, blood clots and blood vessel problems. Living with long COVID can lead to post traumatic stress disorder, depression and anxiety.
Here are the long COVID symptoms you should look out for, according to UT:
Fatigue
Difficulty sleeping
Persistent cough
Shortness of breath or difficulty breathing
Chest pain
Headaches
Joint or muscle pain
Loss of smell or taste
Rash
Hair loss
Rapid or pounding heartbeat
Depression or anxiety
Fever or night sweats
Inability to control body temperature
Constipation
Diarrhea
Memory problems or difficulty concentrating
Dizziness
Confusion
Worsened symptoms after physical or mental activities
Long COVID symptoms can take weeks, months, or longer to go away completely. Initial studies show that most people are improving slowly over time.
If you are continuing to experience symptoms of COVID-19 months after initial infection, speak with your primary care provider about being referred to a multidisciplinary care team with expertise in long COVID.
5. Preventing COVID reinfection is key
Treatment plans look different for each person because it’s based on their specific symptoms. Potential treatment options for long COVID may include a combination of physical rehabilitation, breathing and mental exercises and medications.
According to Dr. Michael Brode, medical director of the UT long COVID program, there’s currently no recognized, FDA-approved treatment for long COVID. Instead, doctors treat the specific symptoms of fatigue, anxiety, shortness of breath etc. For instance, shortness of breath is treated with albuterol inhalers and anxiety is treated with counseling and antidepressant medications. The research team’s goal is to find targeted curative therapies for long COVID.
While long COVID is not as contagious as the initial infection, it is recommended that you receive a COVID-19 vaccination and take the appropriate health precautions to prevent re-infection. The best way to protect yourself and the ones you love is by getting vaccinated, wearing masks and practicing social distancing, Texas long COVID experts say.
