As monkeypox spreads in South Florida, experts have advice on prevention, risk, vaccines
Three days after the CDC issued a health advisory on monkeypox cases in the United States in May, the Florida Department of Health reported the state’s first presumptive case of the viral disease.
A month later, by the end of June, Florida’s case count surged to 73, the third most of any state, after California and New York, according to the Centers for Disease Control and Prevention.
READ NEXT: ‘Absolutely be concerned.’ Monkeypox cases are surging in South Florida
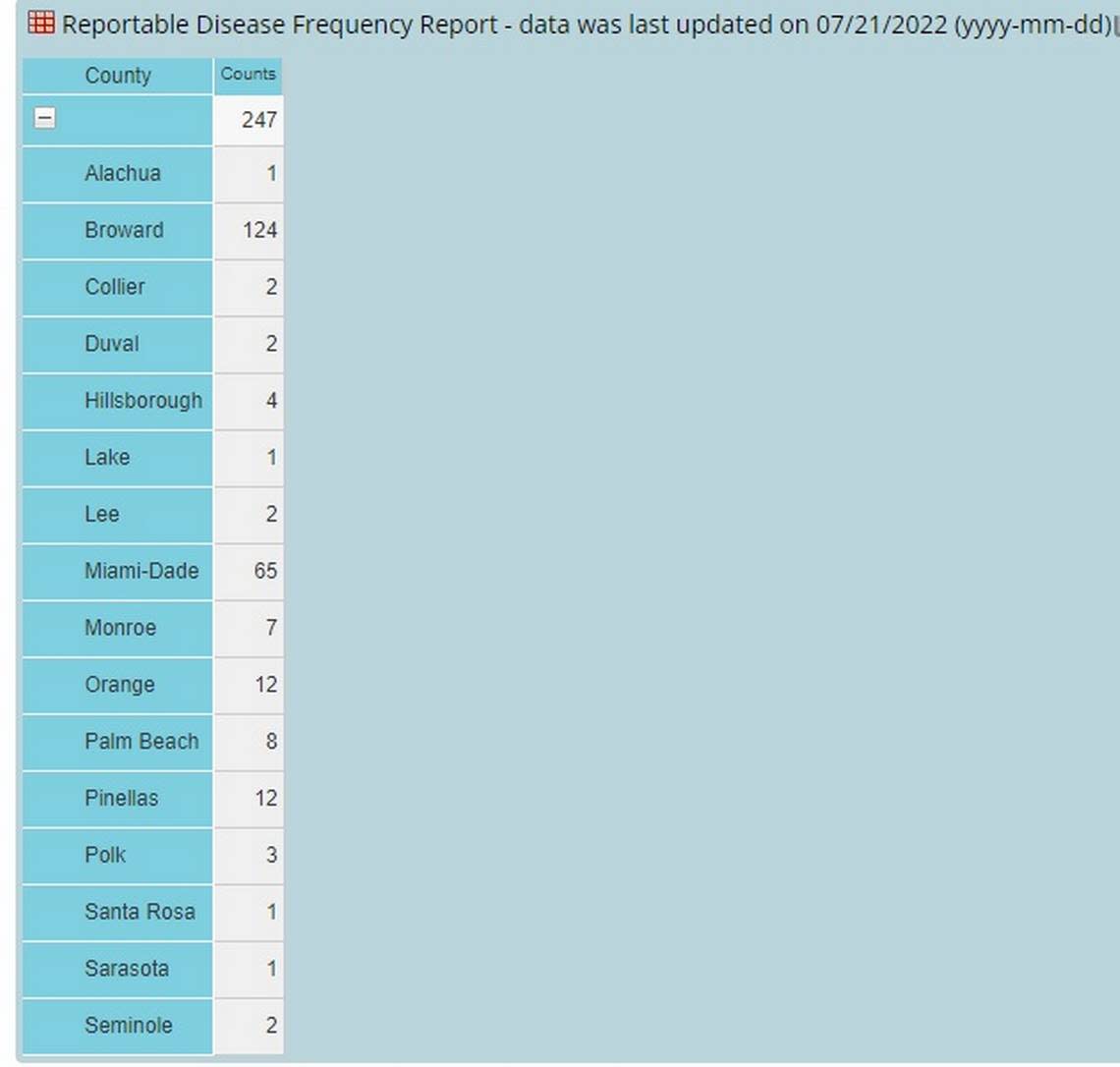
As of July 21, Florida has 247 reported cases, according to the Florida Department of Health, which posts case counts by county. Only New York at 830 and California at 356 outpace Florida, according to the CDC’s states map. Illinois at 230, and Georgia, with 158 cases listed on the CDC map, follow Florida.
South Florida leads the state in monkeypox case counts:
▪ Broward County has more than half the state’s total cases, at 124, as of Thursday, according to the health department.
▪ The more populous Miami-Dade is second, with 65 cases.
▪ Monroe in the Keys reports seven cases.
▪ Palm Beach County has eight cases.
Elsewhere in the state, Pinellas County, which includes St. Petersburg, has 12 cases. Orange County, which includes the Orlando area, also has 12 cases.
Here’s some of the latest information about monkeypox:
How do you catch monkeypox?
▪ Monkeypox is spread by direct contact with the infectious rash, scabs, or body fluids, according to the CDC.
▪ You can get monkeypox from respiratory secretions during prolonged, face-to-face contact, or during intimate physical contact, such as kissing, cuddling or sex.
▪ Handling items such as clothing or linens that previously touched the infectious rash or body fluids can spread monkeypox.
▪ Pregnant people can spread the virus to their fetus through the placenta.
▪ It’s also possible for people to get monkeypox from infected animals, either by being scratched or bitten by the animal or by preparing or eating meat or using products from an infected animal, according to the CDC.
How do you prevent monkeypox?
The CDC offers the following tips on how to avoid catching monkeypox.
▪ Avoid close, skin-to-skin contact with people who have a rash that looks like monkeypox.
▪ Don’t touch the rash or scabs of a person with monkeypox.
▪ Don’t kiss, hug, cuddle or have sex with someone with monkeypox.
▪ Don’t share eating utensils or cups with a person with monkeypox.
▪ Don’t handle or touch the bedding, towels or clothing of a person with monkeypox. If you have to handle these items in your field of work, such as people in the healthcare or hotel industry, minimize skin exposure by wearing gloves and try to avoid pressing bedding linens up against bare skin.
▪ Wash your hands often with soap and water or use an alcohol-based hand sanitizer. (This advice applies to COVID-19 prevention, too.)
▪ If traveling to Central and West Africa, avoid contact with animals that can spread monkeypox virus, usually rodents and primates. Also, avoid sick or dead animals, as well as bedding or other materials they have touched, the CDC suggests.
Is South Florida more at risk?

According to an interview with the Miami Herald in late May, Dr. Aileen Marty, professor of infectious diseases in the Department of Medicine at FIU Herbert Wertheim College of Medicine, said South Florida is vulnerable because the region already has a high incidence of sexually transmitted infections.
Since “sexual transmission is the dominant transmission in this outbreak, the combination of behavior and international travel poses an increased risk for our community,” she said.
What are monkeypox’s symptoms?
▪ Symptoms of monkeypox include fever, headache, muscle aches, backache, chills, exhaustion and swollen lymph nodes followed by a rash.
▪ The distinctive features of monkeypox happen after the first symptoms, FIU’s Marty said. After an incubation period of 5 to 21 days, but usually 6 to 12 days, infected people get early symptoms like a bad headache, fever, back pain, muscle ache and swollen lymph nodes.
▪ These early symptoms generally last one to three days, and then comes the rash.
“The rash is unusual because it classically starts on the face and the palms of the hands and the soles of the feet, followed by rash elsewhere — but in the current outbreak, that has not been the usual spread. In this outbreak, lesions have manifested first in the groin, and the prodrome [early symptom] has not been as severe or notable,” Marty said.
Infectious period
People are infectious from a few hours before the first symptom manifests until the scabs are dry and gone.
According to the CDC, lesions progress through the following stages before falling off: macules (flat lesions), papules (well-defined skin bump), vesicles (blister, filled with clear fluid, usually), pustules (bulging fluid containing pus) and scabs.
The illness typically lasts for two to four weeks. The rash is typically painful, Marty said, and the scabs contain infectious viral particles.
What to do if you have symptoms?
Even if you don’t think you’ve been in contact with anyone who has monkeypox, if you are experiencing symptoms, the CDC recommends that you speak with your healthcare provider to determine whether you need to be tested.
What if you are sick with monkeypox?
▪ Isolate at home if you contract monkeypox, the CDC urges.
▪ If you have an active rash or other symptoms, stay in a separate room or an area that is away from people or pets you live with.
▪ There are no treatments specifically for monkeypox virus infections. But “monkeypox and smallpox viruses are genetically similar, which means that antiviral drugs and vaccines developed to protect against smallpox may be used to prevent and treat monkeypox virus infections,” according to the CDC.
▪ Let your doctor know If you have symptoms of monkeypox. For many, monkeypox resolves in two to four weeks. For others who may be at a higher risk of severe disease, speak to your doctor. You may be at higher risk if you are immunocompromised or younger than 8, or if you are pregnant or breastfeeding, or if you already have skin conditions that can leave you susceptible to further infection.
Is there a monkeypox vaccine?
The CDC recommends vaccination for people who have been exposed to monkeypox and for people who are at higher risk of being exposed to monkeypox.
Two vaccines are licensed by the U.S. Food and Drug Administration and are available for preventing monkeypox infection — JYNNEOS (also known as Imvamune or Imvanex) and ACAM2000.
READ MORE: Here’s where you can get a monkeypox vaccine
Should you still get vaccinated if you already have monkeypox?
“If someone already had monkeypox — rash and fever — the vaccine would likely not help them. It would be too late. The disease would run its course,” said Dr. Mary Jo Trepka, a professor and chair of Florida International University’s Department of Epidemiology at the Robert Stempel College of Public Health & Social Work.
“If someone previously had monkeypox, they would likely have some immunity from that previous infection and that person likely would not be in a high priority group to get the vaccine even if they were a close contact given the restricted supply of vaccine. As this outbreak progresses, we will learn more about the immunity that people develop after natural infection in comparison to the immunity from vaccination,” Trepka said.
When does protection kick in after vaccine?

“The protection you get from vaccination is not immediate. It takes a couple of weeks. In fact, you don’t get full protection until two weeks after the second dose of the JYNNEOS vaccine or one month after the ACAM200 vaccine dose,” Trepka said.
“However,” she adds, “a very important role of the vaccine is in what is called post-exposure prophylaxis. If a person is a close contact of someone with monkeypox and gets the vaccine within four days of exposure, the vaccine can prevent them becoming sick. Even if they get the vaccine between 4 and 14 days after exposure, then the vaccine will likely decrease the severity of their illness. So one of the highest priority groups to get the vaccine are the close contacts.
“When the health department interviews people who have been diagnosed with monkeypox, they ask about the close contacts and then recommend to those close contacts that they get vaccinated if it has not been too long since they were exposed,” Trepka said.
