Medicaid expansion deal reached between NC House and Senate
The House and Senate have agreed to pass Medicaid expansion, reaching a breakthrough after years of debate.
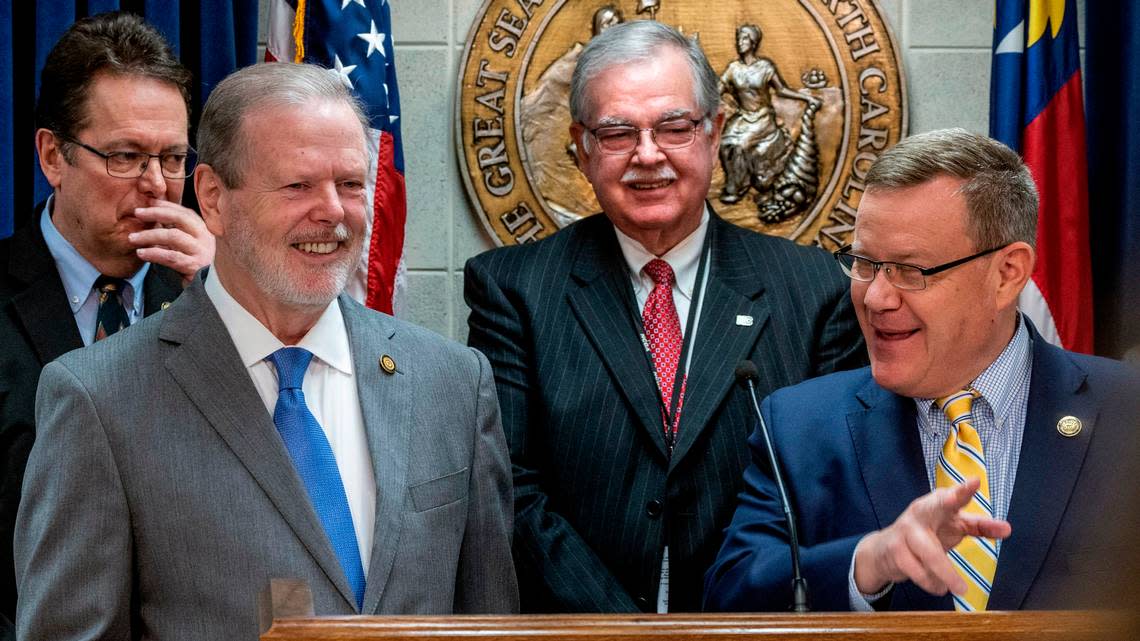
House Speaker Tim Moore and Senate leader Phil Berger held a joint news conference on Thursday at the Legislative Building announcing the compromise between the Republican-majority chambers. Democratic Gov. Roy Cooper has been a longtime supporter of expansion, which would provide health insurance coverage to hundreds of thousands of North Carolinians.
Berger and Moore both said they had not yet talked to Cooper about their expansion bill, but in a statement shortly after the announcement, Cooper wrote that it was “a monumental step” and that he wants it to be written to take effect immediately. Medicaid expansion under a House-passed plan would take effect Jan. 1, but Berger indicated that timing is up in the air.
Moore said the Medicaid bill will “expand access to working North Carolinians. That is going to ensure that there is a more robust supply of a lot of these services. That is going to result in less cost, but at the same time vitally important to protect access to health care, particularly in our rural areas.”
The bill has not yet been filed but will be in the next week or so, Berger said. It’ll have many provisions, some not directly related to Medicaid expansion — including a reduction in “certificate of need” regulations for health care facilities. It will also include a new reimbursement program for hospitals.
“An agreement by legislative leaders to expand Medicaid in North Carolina is a monumental step that will save lives and I commend the hard work that got us here,” Cooper said.
Moore and Berger were planning to meet with Cooper later on Thursday.
Moore said the House and Senate reached the deal late Wednesday night and put the finishing touches on it Thursday morning. He said they “wanted to go ahead and get it out there ... and get the details to to the public, because it’s something we can all be very proud of.”
Medicaid again part of budget talks
North Carolina is one of just 11 states that has not adopted Medicaid expansion under the federal Affordable Care Act, according to research by the Kaiser Family Foundation. The program provides health insurance coverage to certain low-income and needy individuals via state and federal funds.
In North Carolina, childless adults are not eligible for Medicaid, while the current income limit eligibility for a parent or caretaker is 41% of the federal poverty level. With expansion, eligibility would increase to all adults with incomes up to 138% of the federal poverty level.
According to an estimate by the state Department of Health and Human Services, expansion would make 600,000 low-income North Carolinians eligible for the program.
Medicaid expansion has been at the center of the budget process for years. In 2019, a months-long stalemate between Cooper and the General Assembly resulted in no new budget at all. Instead there were several small budget bills.
Medicaid expansion again was part of the 2021 state budget negotiations, but that budget eventually became law without expansion.
It will again be part of this year’s budget process, which could mean that if Cooper wants to sign the budget into law, he might have to make more concessions on policy than if it wasn’t included. The 2021 budget, for example, had a provision limiting the governor’s powers during states of emergency.
Berger said his primary reason for tying expansion to the budget “has to do with matching it up with other money provisions,” and that because the money would be recurring and impact various parts of the budget, “it needs to be coordinated with the passage of an overall budget.”
What’s in the bill
North Carolina’s certificate of need law regulates hospital expansions, new health care facilities, medical equipment purchases and more. It was a big reason Medicaid expansions did not pass in recent years, as the Senate wanted to pass the Medicaid expansion bill with certificate of need changes and the House did not.
The House’s Medicaid expansion bill, passed in February, did not include certificate of need changes, but Berger said Thursday the new compromise bill will.
Berger said the bill’s new version ”will eliminate certificate of need for behavioral health beds, for chemical dependency beds. It will raise the replacement equipment threshold to $3 million and index that number to inflation. It will increase the threshold for diagnostic centers to $3 million and index that to inflation.”
For counties with a population of 125,000 or more, the bill would eliminate certificate of need requirements for magnetic resonance imaging and for ambulatory surgical centers, Berger said. These provisions would become effective years down the line.
These exempt surgical centers in large counties would need to have a specific charity care requirement. Those provisions would not become effective until years down the line, Berger said.
One policy that will not be in the compromise bill is the SAVE Act, a proposal pushed by a bipartisan group of state lawmakers that would grant high-level nurses more independence. The provision was one of many policies tacked on to the Senate’s Medicaid expansion bill last year that did not pass.
Berger said he continued to be supportive of the SAVE Act but that it would not be tied to expansion this year.
“I remain convinced that giving 600,000 people a card that says that their health care is going to be paid for is is going to be somewhat problematic if we don’t increase the supply of folks that can treat them,” Berger said, “We’ve addressed part of that with the CON provisions. I remain committed to working towards the other part of it as well.”
Hospitals were key
Moore said that what had gotten them to this point in negotiations was likely the Healthcare Access and Stabilization Program, which would increase Medicaid reimbursement rates for hospitals.
In a statement, DHHS wrote that expansion and the stabilization program would bring in “$8 billion annually to North Carolina with no additional cost to the state, along with $1.8 billion which can support behavioral health, public safety support, rural health care, and other needs.”
One of the strongest opponents of CON repeal, and therefore of the Senate’s failed Medicaid bill, in the 2021-22 legislative session was the N.C. Healthcare Association, an interest group that represents hospitals.
This year, the group was involved in pushing for the stabilization provision. Last year, the association made an offer for how certificate of need regulations could be changed without being repealed.
The association praised the deal in a statement from Steve Lawler, its president and chief executive officer, who wrote that the “legislation will go far to strengthen the health of people in our state and to support maintaining access to health care, especially in rural communities. We look forward to working with elected officials to support getting this historic legislation passed into law soon.”
Cynthia Charles, a spokesperson for the association, told The News & Observer that while the negotiations on a compromise were between Berger and Moore, “we appreciated that it seems they took the input from our proposal from last fall into consideration as part of the process of coming to an agreement, including on certificate of need changes.”
Berger said this compromise bill was “somewhere between what the hospitals had suggested and what was in the Senate bill” last year.
In a statement, Charles wrote that the stabilization program “gives the state an opportunity to bring in billions of dollars in federal funds to help stabilize rural hospitals and add to the state’s General Fund to address issues such as our growing mental health crisis. This federally funded program comes at no cost to the state and would also have the effects of improving provider participation in our Medicaid program, strengthening network adequacy and access to care.”
Other areas in which the state will save money through Medicaid expansion involve the federal American Rescue Plan Act. The federal government covers 90% of Medicaid coverage costs for the expansion population. Under ARPA, the state’s regular match rate is bumped up 5% over the span of two years, said Robin Rudowitz, vice president at the Kaiser Family Foundation. This is what has typically been cited by lawmakers as a $1.5 billion or so “signing bonus” from the federal government.
Asked about how those additional funds would be spent, Moore said lawmakers “haven’t fine tuned that, but my suspicion is it would be health care related.”