Do you have long COVID symptoms? CDC says 1 in 6 Idaho residents are at risk, what to know
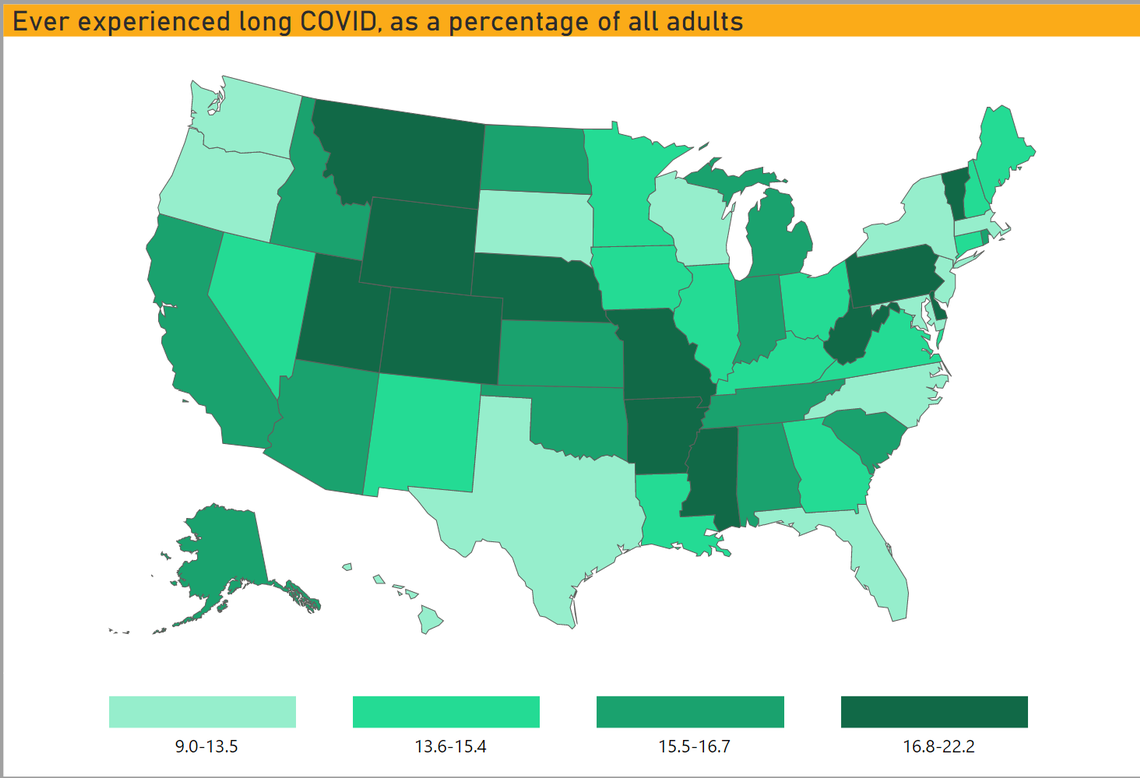
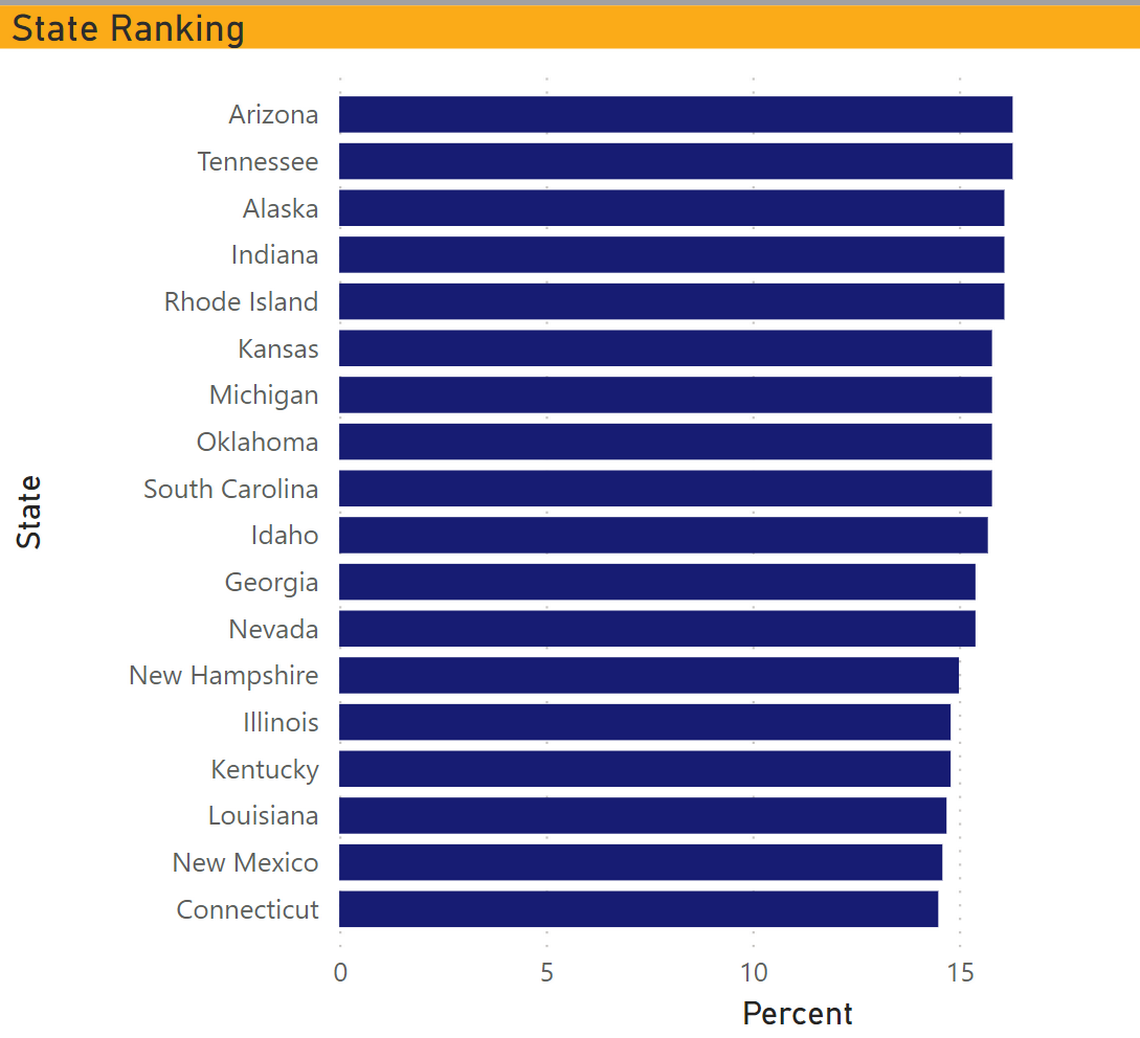
About 15.7% of Idahoans have experienced long COVID, according to a recent CDC survey, slightly higher than the national estimate of 14.7%.
Long COVID, also known as post-acute sequelae of COVID-19, is a syndrome in which people continue to experience symptoms of COVID-19 months after the initial infection. It has been found to impact about 1 in 3 of those who had COVID, and can affect even those who had cases with very mild symptoms.
These are five key facts about the state of long COVID in Idaho.
1. Over a quarter of Idahoans who had COVID also experienced long COVID
An estimated 29.9% of Idahoans who have had the virus have reported experiencing long COVID. That means they’ve had symptoms lasting three months or longer that they did not have before having COVID-19.
Also, 71.9% of Idaho residents with long COVID say that these long-term symptoms reduce their ability to carry out day-to-day activities. Worse, about 22.8% say there are “significant activity limitations.” Some of the more common long-term symptoms include fatigue or brain fog, which is characterized as difficulty thinking or concentrating.
2. Multiple long COVID studies are being conducted
The Idaho Department of Health and Welfare does not track long COVID data. However, the department is following a pair of studies assessing long COVID symptoms.
One study published in the National Library of Medicine looks at the neurological effects and cognitive dysfunction in those with COVID symptoms for more than six weeks. The study found that among 100 non-hospitalized COVID-19 patients across 21 states, 85% reported at least four neurological symptoms, such as brain fog, headache, and taste or smell disorders.
The study also found many patients suffered from non-neurological symptoms, such as fatigue (85%), shortness of breath (46%), chest pain (37%), and gastrointestinal symptoms (29%).
In addition, a second study published in the National Library of Medicine looked at long COVID patients roughly 8.5 weeks after infection. Of the 143 patients studied, 18 were completely free of COVID-related symptoms, 46 had at least one or two symptoms, and 79 had three or more.
3. People with long COVID experience a wide variety of symptoms
Long COVID was added as a recognized condition that could result in disability under the Americans with Disabilities Act in July 2021. The CDC acknowledges that people with post-COVID or long COVID conditions may experience many symptoms and lists them online:
General symptoms
Tired or fatigue that interferes with daily life
Symptoms that get worse after physical or mental effort
Fever
Respiratory or heart symptoms
Difficulty breathing or short breath
Cough
Chest Pain
Heart palpitations
Neurological symptoms
Brain fog
Headaches
Sleep problems
Lightheadedness
Pins-and-needles
Changes in smell or taste
Depression
Anxiety
Digestive symptoms
Diarrhea
Stomach pain
Other symptoms
Joint or muscle pain
Rash
Changes in menstrual cycle
Long COVID symptoms can take weeks, months, or longer to go away completely. Initial studies show that most people are improving slowly over time.
People who continue to experience symptoms of COVID-19 months after the initial infection should speak with their primary care provider about being referred to a multidisciplinary care team with expertise in long COVID.
4. Treatment options for long COVID
Boise State University recommends that individuals with long COVID be referred to healthcare specialists in cardiology, pulmonology, neurology, or other relevant fields. The university also outlines potential treatment options for those with the most common long COVID symptoms:
Fatigue: Patients with fatigue may consider learning the “4 Ps” strategies — pacing, planning, prioritizing and positioning. Undertaking physical activities that involve stretching, strengthening and aerobic exercises can also battle fatigue, but if symptoms worsen, physical activity should be reduced or stopped.
Respiratory symptoms: A primary treatment option is pulmonary rehabilitation, a guided program that teaches individuals to learn breathing techniques and perform breathing exercises.
Cardiac symptom: Those with cardiac symptoms may be referred to a cardiovascular specialist. At-home treatment options will likely involve cardiac rehabilitation, which involves physical activity, education about healthy living, and counseling on removing stress from life.
Neurological symptoms: For patients with brain fog and memory loss, Boise State says doctors recommend exercise and remaining physically active. Those with memory problems can also be taught memory exercises and get in the habit of using memory aids such as calendars and planners.
Psychological symptoms: Individuals who suffer from depression, anxiety, and other psychological symptoms are typically referred for counseling, support groups and medications to manage the symptoms.
Smell and taste symptoms: Boise State experts note that doctors may prescribe topical corticosteroids to reduce inflammation in the nose, which often leads to smell loss. Patients may be referred to an ear, nose and throat specialist if symptoms don’t resolve.
5. Preventing COVID reinfection is key
Treatment plans look different for each person based on their specific symptoms. Potential treatment options for long COVID may include a combination of physical rehabilitation, breathing and mental exercises, and medications.
While long COVID is not as contagious as the initial infection, according to the CDC, it is recommended that you receive a COVID-19 vaccination and take the appropriate health precautions to prevent re-infection. The best way to protect yourself and those you love is by getting vaccinated, wearing masks and practicing social distancing.
