The Little Trick That Could Make Vax Immunity Last Longer

The COVID-19 vaccine was one of the biggest medical breakthroughs in history, but we’re well aware by now that it’s far from perfect. The need for boosters is a sign of the limits of our own immune systems. Whether we get it through vaccination or through surviving a natural infection, immunity can wane over time. But a new study run by scientists in Japan has identified a piece of the immune system that could be a linchpin for designing better vaccines that provide longer immunity from different diseases—from COVID-19 and malaria to many others.
The findings, published Wednesday in the Journal of Experimental Medicine, investigate ways to improve the function of B cells, which facilitate long-term memory against a pathogen. After the body recognizes an infection and fights it off, B cells are taught to remember what these invaders look like and what the recipe is for the specific antibodies designed to attack them.
B-cell education happens in a place called the germinal center, a temporary cell structure housed in places like the spleen, lymph nodes, and tonsils.
We Screwed Up, This Is Really a Three-Dose Vaccine
“A goal of vaccination is to produce high-quality memory B cells for long-lasting antibody production,” University of Tokyo researcher Michelle S. J. Lee, the lead author of the new study, said in a statement. “If you don’t have a functional germinal center, then you will be very susceptible to reinfection.”
Lee and her team were interested in understanding the key factors that help sustain the germinal center—and therefore help maintain B-cell education and function. They had a suspicion that one type of enzyme with known roles in antiviral immunity, TBK1, might be involved.
So the team genetically modified some mice to turn off the function of TBK1 in their B cells, and then infected those mice with malaria (a disease that’s notorious for evading B-cell memory). They found that mice without a working TBK1 enzyme in their B cells were dying more quickly and at higher rates from malaria than their normal counterparts. The few genetically modified mice that survived fought off infection with other kinds of immune responses, but they were very easily reinfected.
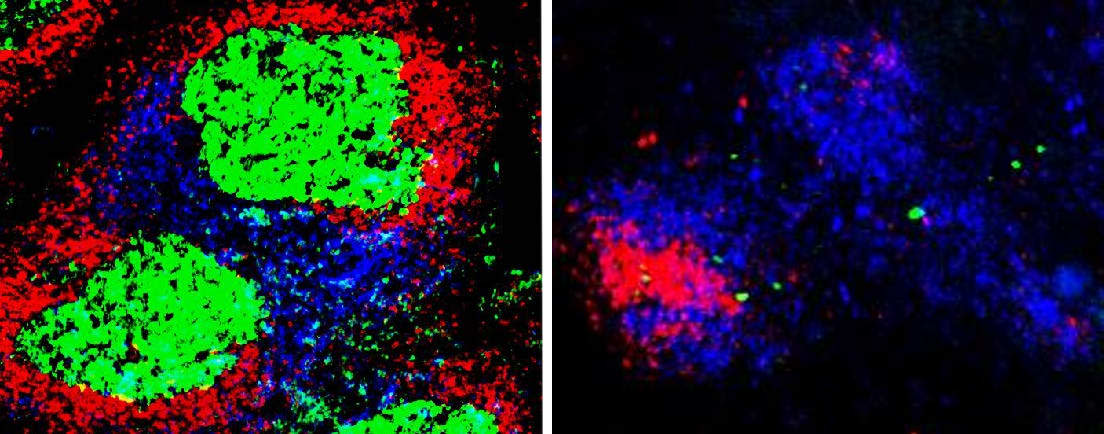
Fluorescent microscopy of T and B cells in mice. On the left, you can see the germinal center forming in the spleen of normal mice infected with malaria. On the right, the germinal center does not form in mice that cannot produce a functional TBK1 enzyme.
Microscopic imaging showed that without TBK1, germinal centers were unable to form—which meant B cells could not mature and retain the kind of long-term memory needed to identify and initiate immune activity against known pathogens. “This is the first time to show TBK1 is essential in B cells to form the germinal centers and produce high-quality, mature antibodies,” said Lee.
What this means is that one very important way we could increase the long-term effectiveness of vaccines is to find a way to amplify TBK1 activity. We could finally surpass the need for boosters and instead rely on a single, supercharged jab. It’s incredibly unlikely we could design a vaccine like this in the short-term against COVID-19. But the findings could be a game changer for improving vaccination against all sorts of existing diseases, as well as how we approach a future pandemic.
In the meantime, get your booster shot.
Got a tip? Send it to The Daily Beast here
Get our top stories in your inbox every day. Sign up now!
Daily Beast Membership: Beast Inside goes deeper on the stories that matter to you. Learn more.
