Racism is rampant in health care and a new memoir reveals how deadly the consequences can be
When Dr. Uché Blackstock left her faculty position in academic medicine four years ago, she had no way of knowing she was making a life-or-death decision. After enduring years of racism and sexism in a toxic work environment, she’d had enough and decided to prioritize her own mental health and well-being.
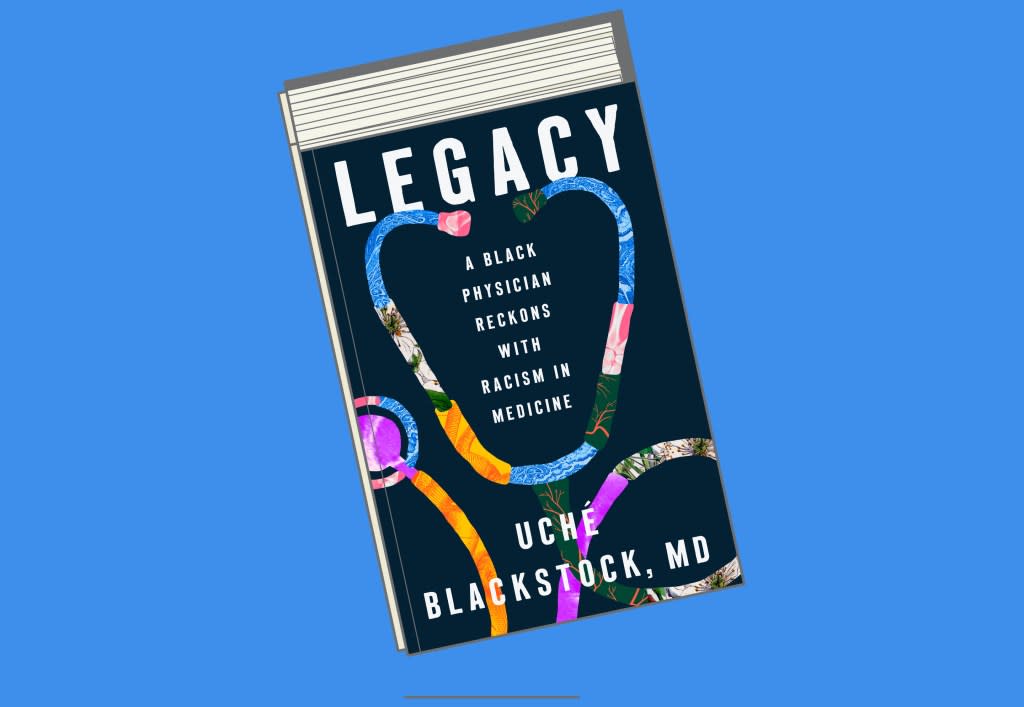
Now, on the heels of the release of her debut memoir, Legacy: A Black Physician Reckons with Racism in Medicine, which also takes a critical look at the intersection of racism and healthcare, Blackstock is grateful she chose herself.
“Best decision I ever made and it’s not lost on me that I was one of the lucky ones to be able to find a way out,” she recently posted on X (formerly Twitter) nearly one week after the suicide of Dr. Antoinette “Bonnie” Candia-Bailey, vice president of student affairs at Lincoln University. “We just want to be able to do the work we love on behalf of our communities in ways that feel authentic to us, where we can speak up about systemic inequities without fear of retaliation, but really it feels like we are asking for too much so we just create our own spaces.”
Which is exactly what Blackstock did in 2019 when she founded her consultancy, Advancing Health Equity, as a way to dismantle racism in healthcare by partnering with health organizations to diversify their hiring and combat racial health inequities. With Black women accounting for less than 3% of U.S. doctors (even though Black people make up 13% of the U.S. population), Blackstock is aware that training more Black physicians is only part of the solution.
“I would love for there to be more Black physicians because that can help to solve the problem,” she says in a video interview with Fortune. “But the other piece of it is we need physicians who are not Black to be able to adequately and competently care for Black people as well.”
This culturally competent care is an important skill Blackstock learned firsthand from her mother, Dr. Dale Gloria Blackstock. Together, with Uche’s twin sister, Oni, the trio became the first Black mother-daughter legacies from Harvard Medical School. Tragically, their mother died from acute myelogenous leukemia (AML) at the age of 47. The experience opened Uché’s eyes to the many ways systemic racism plays a critical (and often fatal) role in the lives of Black Americans.
Studies have shown that people who live in low-income communities, such as the one Uché’s mother grew up in, have higher exposure to toxic environmental contaminants, which can lead to higher rates of cancer. Additionally, as Blackstock writes in Legacy, cancer diagnoses are often delayed for Black patients due to “lack of access to health care and lack of quality, culturally responsive care.”
“Often when people hear these very dismal and sobering statistics about Black communities and health, there is this assumption that there is something wrong with us,” she says. “I need people to see how systemic racism behaves and how it impacts our communities through these practices.”
In a country where Black men have the shortest life expectancy; Black women are more likely to die in childbirth than any other group and Black babies have the highest infant mortality rate, Blackstock is committed to shining a light on the deep inequities that exist in the U.S. healthcare system. Although she’s crystal clear that it is not on Black people to fix a problem we didn’t create.
“Sometimes I think it’s easy for people to see interpersonal racism, like when someone is called a racist slur or mistreated because they’re Black,” she says. “It’s something entirely different to see how policies our own federal government sanctioned and created have led to racial health inequities. Once you’re able to connect the dots, it’s very hard to unsee them.”
Indeed, the Centers for Disease Control and Prevention has acknowledged that social determinants of health, such as housing, education, and employment, are “key drivers of health inequities within communities of color, placing those within these populations at greater risk for poor health outcomes.”
And it should not rest solely on these communities to fix a problem we didn’t create, as Blackstock is calling on elected officials, non-Black allies, healthcare institutions, medical schools and academic medical centers, as well as white physicians and healthcare professionals to reevaluate the processes and procedures that led to these injustices.
“It’s not just about writing a prescription. It’s not about telling someone to exercise. Because how can someone exercise if they don’t have the green space in their neighborhood or don’t feel safe in their neighborhood to exercise?” Blackstock asks. “Physicians need to understand the context in which their patients are living, playing, praying and being. They need to understand all of that.”
This story was originally featured on Fortune.com
