Measles has been eradicated in the U.S. for 24 years. The number of cases this year may change that
Since the start of 2024, there have been 113 cases of measles in the U.S. and seven outbreaks, concerning public health officials. As the highly contagious virus continues to spread, being familiar with measles rash images and other symptoms, along with vaccination and other precautions, can help keep you safe, too.
Measles has been considered eliminated in the U.S. for over 20 years, meaning it is no longer constantly present, though there have been small outbreaks.
]However, the growing number of cases in 2024 is threatening to overturn this status, the U.S. Centers for Disease Control and Prevention said in an April 11 report. At least 17 states have reported cases of measles since the start of the year.
Childhood vaccination rates are falling, and cases have been rising for several yers. Now, the CDC is urging people to get immunized against the measles, as the vaccine is highly effective. Over 80% of people who've gotten measles this year were either unvaccinated or their vaccination status was unknown, NBC News reported.
In order to prevent measles outbreaks, at least 95% of the population must have received two doses of the vaccine. But two-thirds of U.S. states have not hit this mark, TODAY reported in a segment aired Feb. 22.
Globally, measles cases were up 79% in 2023 compared to the prior year, according to the World Health Organization. In a press conference on Feb. 20, WHO noted that by the end of 2024, more than half of countries would be at risk of a measles outbreak unless prevention measures are put in place.
“Measles is a highly contagious virus that can spread quickly through the general public if people are not vaccinated,” Dr. Sandra Kemmerly, infectious diseases specialist and system medical director for quality and patient safety at Ochsner Health in New Orleans, Louisiana, tells TODAY.com.
So, what does a measles rash look like? How can you identify measles symptoms and how long are you contagious? Where is measles spreading in the U.S.? How long is the measles vaccine good for? Here's what to know.
Measles hits the US in 2024
So far in 2024, there have been at least 113 cases of measles and seven outbreaks in the U.S.
Measles was declared eradicated from the United States in 2000 due to a highly effective vaccination program.
“Over the last decade and a half, we saw an irregular but overall increase in the number of cases,” Dr. Linda Yancey, infectious disease specialist at Memorial Hermann Health System in Houston, Texas, tells TODAY.com.
The trend stopped abruptly in 2020 when the COVID-19 pandemic hit as everyone was isolating and protecting themselves against the coronavirus, she adds. But now, the U.S. is again seeing a rise in cases. Many people have missed vaccinations due to the COVID-19 pandemic, and anti-vaccination sentiment is on the rise, NBC News reported.
Worldwide, there are currently large measles outbreaks in many Asian, Middle Eastern, African and European countries, a CDC spokesperson tells TODAY.com.
Where is measles in the US?
So far, the following U.S. states have recently reported cases of measles:
California
Georgia
Missouri
Maryland
New Jersey
Ohio
Pennsylvania
Washington
Arizona
Minnesota
Florida
New York
Virginia
Illinois
Indiana
Louisiana
Michigan
Is there a measles outbreak in the US right now?
So far in 2024, there have been seven measles outbreaks in the U.S. That's compared to four outbreaks reported in all of 2023. An outbreak is defined by more cases occurring than what’s expected, according to the CDC.
“There have been a few small, isolated outbreaks mostly related to international travelers and children who have not been vaccinated,” Kemmerly explains. “Infectious diseases experts are on high alert.”
The last major outbreak of measles in the U.S. occurred in 2019 when there were 1,274 individual cases confirmed in 31 states, according to the CDC. This was the highest number of reported cases in the U.S. since 1992, with most cases among those who were unvaccinated.
Why is there a measles outbreak?
The decline in measles vaccination rates globally increases the risk of larger measles outbreaks worldwide, including in the United States, a CDC spokesperson explains.
“Because measles remains a common disease in many parts of the world, we are seeing cases brought into the United States by unvaccinated U.S. residents following international travel,” the spokesperson adds.
As the COVID-19 pandemic caused many children to miss their well visits, fewer children were vaccinated compared to before the pandemic.
The CDC estimates over 61 million doses of measles vaccines were either postponed or missed from 2020 to 2022 due to the pandemic.
“When community protection drops, we know that unvaccinated people are at risk,” a CDC spokesperson says.
The pandemic also fueled the anti-vaccine movement — despite infectious disease experts and health officials emphasizing to the public that vaccines are safe and prevent disease.
Last year, the CDC also found school vaccination exemptions were the highest on record among kindergarteners, with measles vaccination rates lower than pre-pandemic levels at 93.1%.
Experts say this is below the 95% threshold needed for herd immunity for measles, where enough of a population is vaccinated so that even if some get measles, outbreaks cannot occur.
“The current increase in cases is alarming and can most likely be explained by a decrease in the overall vaccination rate,” Kemmerly says.
What are the symptoms of measles?
Measles has several stages of infection that occur over two to three weeks.
The incubation period, or the time between exposure to a disease and symptoms starting, is usually one to two weeks. Symptoms then develop in stages, lasting about 10 days in total. Recovery also progresses in phases.
The first symptoms of measles last two to three days and are non-specific and mild, including:
Cough
Runny nose
Watery eyes
In the next phase, look for:
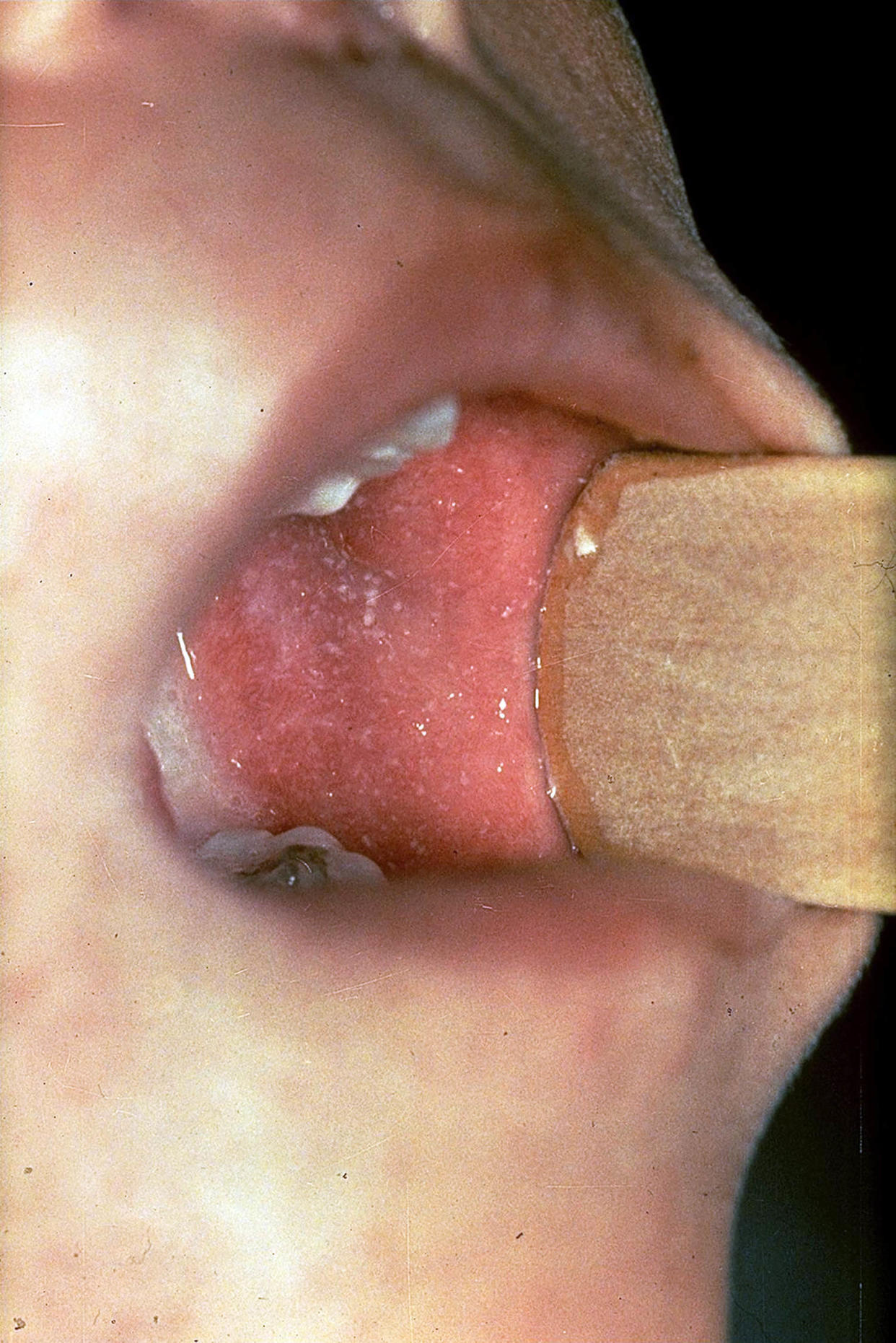
White spots in the cheeks called Koplik spots.
A red rash, usually three to five days after the first symptoms develop.
A high fever as the rash starts to appear
Muscle pain
Sore throat
Usually the rash lasts about a week. You’ll know you’re recovering if:
The rash gradually fades.
The cough goes away.
The skin peels.
Measles symptoms in adults versus kids
“Kids and adults will have a similar pattern of symptoms,” Yancey says.
But some children, especially those not up to date with their vaccines or younger than 5, are more likely to experience complications, such as ear infections and serious infections, such as pneumonia and encephalitis, a life-threatening inflammation in the brain.
Approximately, one in five people with measles is hospitalized, according to the CDC.
What does a measles rash look like?
A measles rash is the most prominent symptom of the virus. It tends to develop three to five days after the first symptoms, which usually resemble a cold.
Here are some specific characteristics and pictures of measles that can help identify whether you have a measles rash or something else.
White spots over a red background inside the cheeks (Koplik spots). These skin findings are unique for measles, so if you see these lesions, it’s most likely measles and nothing else.
A red rash that looks like small raised bumps. These erupt on the face and near the hairline, then spread down to the rest of the body.

The rash's bumps will eventually cluster together, giving a “splotchy red appearance” all over the body, according to Mayo Clinic.

The rash will gradually fade first on the face and last on the extremities.

After the measles rash faces, the skin will peel where it was for about 10 days.
What other illnesses are mistaken for measles?
Measles symptoms can resemble numerous other illnesses depending on the stage of the disease.
Early stage
In the early stage of the illness, measles share symptoms with common childhood respiratory conditions, such as:
The common cold
The flu
Respiratory syncytial virus (RSV) infections
One clue measles is the most likely diagnosis is high fevers.
Rash stage
The classic sign of measles is a red rash that spreads all over the body, but this type of rash, described as morbilliform, is common among many other conditions, especially viruses, bacterial infections and autoimmune disorders.
A measles rash can also look like a drug rash, which develops after taking a prescription medication, usually on the chest and abdomen. It may itch but will go away after stopping the medication.
Viruses with symptoms similar to measles:
Rubella (milder symptoms that last only several days)
Parvovirus B19 infection (“slapped cheek” rash on the face followed by a fine lacy rash on the body)
Roseola (rash develops after fevers disappear but child appears well)
Infectious mononucleosis or “mono” (sore throat, fever and enlarged neck lymph nodes with red blotchy rash on the body)
Hand-foot-mouth disease (sores in mouth and rash on hands and feet)
Dengue fever (fever, headache, pain behind eyes and joint pain with red rash that appears like “white islands in a sea of red” after international travel)
Bacteria infections with rashes similar to measles:
Scarlet fever (flu-like symptoms, then pink or red rash that feels like sandpaper)
Meningococcemia (life-threatening infection associated with pinpoint purple spots that stay present when pressed)
Rocky Mountain spotted fever (splotchy red rash after a tick bite that starts on the wrists and ankles, then moves inward to the trunk)
Autoimmune diseases with a measles-like rash:
Henoch-Schönlein purpura (abdominal and joint pain associated with a purple rash that looks like bruises, often on the legs and buttocks)
Kawasaki disease (fever, red eyes, red cracked lips, enlarged lymph nodes in neck, swollen hands and feet)
Multisystem inflammatory syndrome in children, aka MIS-C (fever with severe illness resembling symptoms of Kawasaki disease after COVID-19 infection)
Since they are so many possibilities of the rash, doctors must confirm a suspected measles case with testing.
Is a measles rash contagious?
Yes, a measles rash is contagious. The virus is one of the most easily spread in the world, passing from person to person through the air with talking, coughing and sneezing.
People are generally contagious from four days before the rash develops to four days after, the CDC notes.
You can spread or contract measles from someone by:
Sharing food or drinks
Kissing
Shaking or holding hands and hugging
Touching a surface with the virus and touching your eyes, nose or mouth
During pregnancy, childbirth or nursing
How long is the measles vaccine good for?
Receiving two doses of the MMR vaccine as a child according to the recommended schedule is good for life, meaning you do not need a booster, according to the CDC.
The MMR vaccine protects against three infectious diseases: measles, mumps and rubella.
Typically, children get two doses early in life, starting the first dose at 12 to 15 months and the second dose at 4 to 6 years old (but they can receive it earlier as long as it's at least 28 days from first dose).
Adults who are not immune should get at least one MMR vaccine, but those who are at higher risk of contracting the disease, such as college teachers, health care workers and international travelers, should get two vaccines at least 28 days apart, according to the CDC.
The vaccine is “highly protective," the CDC emphasizes. “One dose of the MMR vaccine provides 93% protection against measles and two doses provide 97% protection,” a spokesperson explains.
For those who are unsure if they are immune to measles, the CDC says there are three main ways to find out:
Lab test: Ask for a blood test that looks for antibodies against measles. If the test is positive, this means someone was naturally infected in the past or were previously vaccinated.
Birth year: Adults born before 1957 are presumed to be naturally protected against measles (because they were infected as a child).
Written documentation: Adults not at high risk for exposure and preschool-age children are considered immune if they have at least one documented dose of a MMR vaccine that was given on or after their first birthday. Adults high risk for exposure and school-age children need two documented doses of the MMR vaccine to be presumed immune.
Who needs the measles vaccine?
Children, students in post-high school educational institutions, adults and international travelers need the vaccine, according to the CDC.
Children and students should receive two doses, while adults who were not vaccinated as kids or are otherwise immune typically need one. However, if as an adult, you work with students, travel internationally for work or are a health care provider, the CDC recommends two doses.
Women of childbearing age who are not immune to measles should consult their doctors about the vaccine if they have plans to get pregnant, per the CDC.
How long for measles to go away?
Since there's no cure for measles, it has to run it's course which typically takes 10-14 days, per the Mayo Clinic.
To alleviate you symptoms, focus on hydration, rest, pain killers for discomfort, gargling with salt water and isolating so that you don't infect others.
This article was originally published on TODAY.com
